Month: September 2021
The Ultimate Guide To Stopping Low Back Pain
The Ultimate Guide To Stopping Low Back Pain
In less than 20 minutes you will learn the in and outs of lower back pain while Sherlocking your way to determining myth vs truths on the best ways on how to stop back pain.
Why?
Well, you are here probably because you have had back pain or someone you know has and this obviously interests you enough otherwise you would not be here. So grab a cup of coffee or beer (depending on what time of day it is, no judgment) and let’s dig in.
The Ultimate Guide To Stopping Low Back Pain
As stated in the 2018 Lancet Journal publication series on the epidemic of lower back pain, nearly 80% of individuals will have some sort of lower back pain in their lives and it is estimated that roughly 30-40% of individuals have some form of lower back pain right now.
In short, it seems to be important and it seems that many people are dealing with it.
So in conjunction with the conclusions from the Lancet as well as many other resources we have boiled this complex issue down as best as we can to try and help you and your loved ones overcome what sometimes feels like an overwhelming issue.
We hope that if anything you can gather one piece of valuable information that will teach and highlight something about your body that you did not know before, so that you can stop your back pain.
This is so important for me to share with you because I was where you are, and the cookie-cutter approach did nothing for me until I took all of the information from many different resources and started putting the pieces together for what my body needed. Of course everyone had their own take on how to stop back pain, and their way was better than the rest. Now this is usually best managed with a professional such as a great chiropractor or physical therapist (that I will again argue does not do a cookie-cutter approach unfortunately with how well people market this day will lie about what they do, so reach out if you need a referral!)
The journey on how to stop back pain will always begin by determining when did the pain started? Keep in mind while this provides us with a good amount of information, the issue may have started in the past when you did not have pain and we are simply just seeing it surface now that is why a proper history and examination is needed [just taking X-rays is not an examination].
If you have ever been to any sort of provider in the past this is the first question they will typically start with.
Asking when the pain began along with how will give you a great deal of information as to what might be going on and how serious your pain might be.
When discussion how to stop back pain we must remember that less than 1% of lower back cases are related to some sort of serious pathological issues such as cancer, tumor, and infections, etc…
This is important to know because all too often many of us jump to worst-case scenarios because our back really hurts and we figure we must be dying. Be rest assured it can heal and you will too.
So what does this leave us with then…
Well if it started a long time ago and it came out of know where we can dive in and find out what it triggering it and get you to move a littler differently and have great results. We can also have great results if it just started not that long ago and you know that you might have picked up a weight wrong or your child. All of this sets the groundwork for teasing out what are the true underlying causes of the pain you are experiencing.
One analogy that I always use when discussing this with my patients and clients is: if there is no trauma that occurred when your pain began there is most likely a reason as to why it started and we can figure out what that is to help with the current pain you are having and more importantly allows us to prevent or reduce the chances of it happening again in the future.
Diving in deeper for future conversations we will go over the pain model and how different psycho-social factors will also play into how we perceive pain. Ultimately we must appreciate that we having a discussion on how to stop back pain, it is wise for us to understand the full picture. It is not as simple as just saying your back is our of “alignment” or your pelvis is “torqued”.
What is the current management strategy for the majority of back pain?
Wait it out, and if you want to be a little proactive about it:
- Rest
- Ice
- Pain medication
- Stretches
- Surgical consultation
When having these discussions with our patient about how to stop back pain we cannot argue that time will help! But most of us, especially those that are here reading this want more and want to return back to their sports, fitness, or active lifestyle so we have to be a little more progressive in our thinking and approach. (Let me clear the air by saying all of the above bullet points will also work, and they might work for you, but it is better to determine who and why rather than a blanket approach for all!)
Below we will review the 10 myths and 6 truths about back pain and how you can successfully recover, feel stronger, and teach you how to stop back pain.
The 10 Myths About Back Pain
- Rest is best; sit back and wait
- Your back is weak
- You need X-ray or MRI to fix pain
- You will have back pain the rest of your life
- Core strengthening is overrated
- Your parents had back pain you’re doomed
- How you move has nothing to do with pain
- How you sit does not affect your pain
- You won’t be able to play or pick up your kids or grandkids
- You will always have to do your back exercises
The 6 Truths About Back Pain
- Your back is strong
- Movement will help
- Sex can still be enjoyable
- Let your body heal and it will
- Audit your lifestyle and what is important
- Deadlifts are good for you back
We are going recap on Myths and Truths and What to do Next. Many of you will be encouraged to jump ahead to what to do next part and I completely understand why. But hang on with us and read through the whole article, because I guarantee the you will discover something that will be the missing link for you based on what you might have been told before in the past so that you can finally take control of what has been robbing you of so many things in your life. The missing links will help you de-code what you should be doing in the future to eliminate pain, get stronger, and move better!
Continue on To The Ultimate Guide To Stopping Low Back Pain
10 Myths on How To Stop Back Pain
1. Rest is Best; Sit Back and Wait
Yes, sometimes rest can be beneficial for your back pain. But we need to redefine rest… Typically when practitioners are telling you to rest they mean, and or it is understood by the patient, to simply wait and do nothing and things will run its course and things will get better. So individuals will stop what they are doing which typically leads to sitting around on a couch doing nothing and waiting.
This is the opposite of what we want to be doing!
We want to move! Your body wants you to move!
Now, what we need to understand though is it matters how we move. With everything, we insert in context. The context might be the single most valuable piece of information to determine how your recovery process will be.
What your feeling and how you’re experiencing your pain and discomfort might be completely different than someone else, and I am here to tell you now that everyone has a “high pain tolerance”. We are not downplaying by any means what you are experiencing and certainly not dismissing how bad your pain might be. Your pain is your pain and what you are experiencing is real to you so we meet you where you are at, and any great practitioner should be doing the same with you.
Back to sitting and waiting… We have had individuals basically crawling into our office because there pain is so bad and others who are fine but in certain positions or contexts their pain is excruciating. Meeting you where you are at, we need to determine the best movement context or code for you.
For some this might be standing in one place and shifting your hips forward and back, for others it might be laying on your belly and propping yourself up on your forearms, we might suggest you got for a brief walk or perform bodyweight air squat, and for other we might simply say keep training or working out just reduce your load.
One of the more important reasons we also encourage movement and reduction of sedentary positions in the increased inactivity of certain muscle groups as a result of pain as seen commonly in the glute complexes and lumbar paraspinals. These same muscle groups are commonly seen to be dormant in sitting postures or positions. These same muscle groups are vital for stabilizing and controlling the lumbar spine and lower back. So, in essence, the more we sit we are encouraging more complacency in these muscle groups instead of encouraging more activation which is ultimately what movement with encourage.
Determine the hardest thing you can do reasonably well and with limited pain and do it over and over again. This is how we wait! We wait by encouraging the body to move yet respect the protective mechanisms that it is going through.
In doing so you will find that your pain will diminish quickly and you will be able to move around staying active in your life, work, and be proactive with your health.
“A body in motion stays in motion, and a body in rest stays at rest” -Einstein
2. Your Back is Weak
Your body is strong! Do not let anyone tell you otherwise.
Could we be stronger, maybe, but don’t assume that because your back is hurting that it is because your back is weak and fragile. If you could actually see how much force and generated and controlled with your lower back you would actually be amazed. So let’s squash that here and now!
More importantly, we must understand more about the context of your pain and how, when, and where did you start to feel the discomfort.
Many times the activities or movements we are performing might be above our capacity or threshold so we start to develop some pain or discomfort but that does not mean it is weak, it simply means we are doing too much for it and or we need to create more resiliency!
A weak back or a weak core is often to blame for the symptoms we are experiencing, which is confusing when we are prescribed strengthening exercises. But recall that our body adapts and the adaptation come from stress being put upon the body.
Stress or load > capacity or tolerance may result in injury or pain
But if your capacity/strength/tolerance > than the stress imposed upon your body, then you get stronger.
By simply redefining what we mean by weakness, strength, capacity, and load you can gather a better appreciation for what your body can actually do and be motivated to make it the best damn back you have ever had. I mean you pretty much owe it to yourself to do so, and what is great is that it will thank you by feeling great and performing at the top of its game whenever called upon.
I cannot think of a better relationship than that if you ask me
Trust in it and it will reward you!
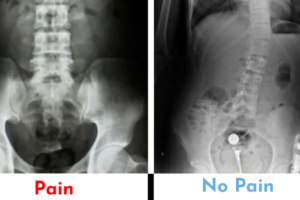
3. You need an X-ray or MRI to learn how to stop back pain
One of the most over-prescribed medical interventions in today’s society is medical imaging. It is believed the be the gold standard for treatment because we can see what is going on in the inside of the body and the tissue structures associated with the pain we may be experiencing.
While the breakthrough of medical imaging has been revolutionary for modern medicine and something to this day that our clinic and progressive colleagues will still prescribe, it is being overused and used more as a fear-based tool than educational component.
This is especially true for the case of lower back pain!
Let us paint a picture of a specific example of how this plays out…
An individual in their 50s present to an orthopedic office (and we have seen this exact same scenario played out at chiropractic office, urgent care, or ER settings, and Primary Practice) with acute lower back pain that is intense and debilitating making it hard for them to walk or more. While they have reported some lower back tightness in the past from working as a landscaper they have never reported really any pain in their lower back, despite all the years of hard work. Now recall that the pain just start and they have not had pain before… They get an x-ray to determine what might be causing the pain they are experiencing at the office. The provider evaluates the images and sees boney changes that one would not normally see on a “healthy spine” (I cannot make the air quotes any bigger, although I wish I could because there is no such thing as a “healthy spine”!). Because of the osteoarthritis, they see on the plain film X-rays the provider determines this much be the cause of their pain.
Now even those that are not providers when I ask them can agree that these boney changes cannot happen overnight but yet their pain pretty much started overnight. So if they have had the boney changes prior to and after the pain they are experiencing (remember it will get better) then we can pretty much assume that the boney changes are not causing the pain because they are always there and have been there.
Here is a perfect example of how medical imaging was used as the first line of treatment rather than a proper evaluation and questionnaire to determine what is actually triggering the pain and why it began in the first place.
This same story is played out for MRIs as well.
The patient-centered approach has clearly determined that conservative treatment methods and active care protocols should be used first and if conservative care options have failed then perhaps medical imaging should be considered (I would encourage a second opinion in your conservative care as well before exploring imaging if you have not been seeing your results)
Now it must be said that imaging can still be valuable and we will use that information in the whole process of gathering data to best determine the appropriate path for you, it cannot be the stand-alone piece of evidence that would suggest the best route for you.
4. You will have back pain for the rest of your life
How sad and frustrating does this sound?
If this was your first episode of lower back pain and you were just told this, you might be having a number of different thoughts rolling through your head right now. And we can see how the psychological side of pain can come into play.
Who do we commonly hear this from?
- Practitioners
- Family Members
What if instead, we change the narrative slightly…
Can you stay with me for just a minute because this can be very powerful for you or another family member/friend?
How we approach this in the office:
“You know what, Miss Jones? Back pain is fairly common and there are obviously various forms of back pain and underlying causes to your pain. The likely hood that the pain is caused by something serious is well under 1%. This means that although we have pain right now, you will get to the other side, and with our guidance and direction you will have a better understanding of what might have caused the pain, how you can be in control of your pain, and ultimately how you can manage any potential flare-ups that might happen in the future. Now I don’t know about you but when I know I have a little more control in my life, my stress levels go down, my pain goes down, the likelihood of me getting into more sports and activities go up, because I know what to do and how to do it, and you know what if you have some questions or you need a little more TLC you can come right back here and we will help you along the way! If we can make you a little stronger and a little better than before, do you think that might help your pain? Would you be interested in investing in yourself to get there?”
Or something like that.
Key Points:
- Very unlikely your pain is caused by something very serious
- You will get better
- Guidance and direction to help you become more self-dependent
- Understanding what and how has profound impact for tackling future potential flare-ups
- Better understanding and awareness = Freedom and Independence
- Need a little more help? We got you!
- Become more resilient
5. Core strengthening is overrated
Often times this term of “core strength” gets thrown about to easily without really any context or direction as to how this might be important for someone.
In the argument for back pain this is all too common. Recommendations are usually:
- You need to strengthen your core
- Core strength doesn’t matter, this is caused by something else
To help clear the muddy waters as it pertains to core strength we should rephrase the term “core strength” to “torso control”.
Why is torso control important for back pain?
Well… the back is kind of attached directly or even considered to be part of the core/torso so I can confidently say that there are probably a few good reasons as to why we should be exploring torso controlled movements.
A few basic key points of why we do torso controlled movements (core exercises):
- It activates and helps the stabilization response of the muscles responsible for torso control
- It strengthens the muscles of the torso (use muscles they get stronger)
- Bring better body awareness to the area to promote more effective movement and control
- Creating a stable core prevents excess lower back motion and energy leaks when exercises or lifting weights
- Provides a stable platform for the big greasy joint like the hips and shoulder to push and pull off of
To sum up, everything goes through the torso to some level or capacity and if we have pain, weakness, or a lack of control and stability we will see energy leaks and decreased efficiency and/or we might see a lack of load transfer which in turn relates to load absorption into the lower back.
How are these applied working with Live LOUD?
We start with where you are. If you are in acute pain there might be a few movements that help you reduce your sensitivity first and foremost, and then we build off of the most difficult thing that you can do well. Then we progress, we keep the needle moving forward until you are able to do confidently all of the things that you want to be able to do.
Plain and simple, no gimmicks, straight forward.
Now one thing we will always emphasize is the devil in the details. Notice we said “simple” and not easy. All too often these basic building block movements are botched and have little to no effect and or might even be potentially harmful to our situation.
SCHEDULE NOW IN OFFICE OR FOR A TELEHEALTH SESSION TO DISCUSS YOUR LOW BACK PAIN
6. Your parents had back pain–you’re doomed!
There are so many fascinating aspects of the human body. Epigenetics is by far one of the most intriguing areas of interest that literally blows my mind when topics arise for discussion. That being said we do know there are some familial ties to our back pain.

All too often we hear, “Well, you know my mother had back pain and she always talks about it and says to me, I just hope you do not get back pain as I have, it is just horrible.”
If we put that into context we can see how strong of an influence that might have on someone especially if they start experiencing the slightest bit of pain, and that mentality confirmed through practitioners not empowering the opportunity in front of them but simply reflecting on a past situation that was completely different than their own.
So yes there may be some influence as to why you may be experiencing some back pain if your parents have had it in the past, but we again default to the process of rectifying and coming up with a solution based on where you are and your goals. We note that a family member might have had pain but it does not honestly hold much if any ground as to what we will do for you.
You present to us uniquely in your own and we will focus on the solution based on that solely.
7. How you move has nothing to do with your pain

This one is a loaded myth! And rightfully so there are a few solid arguments as to why that may be the case.
BUT!!!!
Just as we stated before and will again now and in the future. CONTEXT!!!
There are a few ways of dissecting this argument and we will start with the present because that is where we are living. Let us say for instance you have pain right now. And there are certain positions or ways in which you move that increase your pain or discomfort and certain ways the alleviate you pain or discomfort.
(for literally everyone this is true to some capacity)
Thus we can deduce that how you move has something to do with the pain that you are experiencing correct?
Perfect, problem solved. NEXT!!
If we expand upon this we can use the example of a cut or lesion on the skin over a knuckle. Now for anyone who has had this before you can attest that this sucks and is nearly impossible to heal, until you naturally start to realize the movements the open the wound and the movements that promote healing. Just as we did in that example we use the same thought process to promote healing in the back and reduce prolonged recovery. If a movement hurts then we either need to remove it or modify it so it does not hurt. We prevent the picking of the “scab” and the healing process naturally will occur!
Now we must evaluate the past and the future and come to some potential conclusions.
Might our movement behaviors in the past influence how we have gotten ourselves into this situation?
Some will argue yes and some will argue no.
I am radically in the middle!
But I swing to the yes… why because we are creatures of habit and our movement patterns follow this behavioral pattern leading to repetition after repetition of load bearing movement on tissues that have limited capacity.
“It is not the load that breaks us down, but the load that we are not prepared for” -Tim Gabbett
Our bodies will heal and recover and become more resilient but if we are doing the same thing time after time and not letting that adaptation process properly happen, then we run the risk of injury or tissue damage.
GREAT NEWS THOUGH!
You can also heal from this as we had said time and time again.
SCHEDULE NOW IN OFFICE OR FOR A TELEHEALTH SESSION TO DISCUSS YOUR LOW BACK PAIN
8. How you sit has nothing to do with how to stop back pain
Unfortunately, it seems to be such an ingrained part of our society today, but the majority of us are sitting too long and not moving enough.

Take into consideration the multi-million dollar business or ergonomics.
Now while I will agree with some of the products out there many have no benefit to the general consumer and simply utilize that term for marketing and advertising to increase sales.
That being said what should we do?
Well following many of the recommendation from up above we need to consider the directional preferences of you pain and which positions feel better and which positions feel worse.
Simply put, try to do more of the good and less of the ouchy bad.
Easier said than done right.
So what might we do?
Use some tools to help you remain in the positions and postures as well as reduce the muscular activity needed to perform them to allow for longer times in those positions.
Then add micro-breaks, if you sit for a job I want you up and our of your chair moving for at a minimum 1-2 minutes every 20-30 minutes!!!
Tools to help:
- Yoga wedge to sit on and roll pelvis in ideal position
- Rolled up towel to sit on and roll pelvis
- Sit at the front of the chair and roll pelvis
- Stability/Yoga Ball
- Sit all the way back in the chair and use a lumbar support
Just as we stated above this allows you to take a commonly painful activity, such as sitting, and reduce the sensitivity that is imposed on the back to allow the feed-forward loop we are trying to initiate to take place. Keep in mind this is more directed towards if you are actively having back pain and sitting flares you up.
Those that might be experiencing back pain from sitting might just need to get up and move. Pain does not equal harm, and the discomfort you are experiencing more likely than not is simply a trigger to get you ass up and moving!
9. You won’t be able to play or pick up your kids or grandkids
As a parent now I can confidently say this one is tough. And I myself have had an episode where my back locked up on me and it was very challenging to help around this house, help with the kids, and really do much of anything.
But I trusted to process and from not being able to walk to the bathroom or put pants on very well, a week later I was deadlifting from the ground again building up my foundation.
Now, this all comes back to building resiliency and expanding our foundational base.
We know that a pyramid height is controlled by the based.
If we are able to expand our foundational support we will not only have a better platform for future progress, we will also find that we do not fall that far when we have a setback.
Whereas we can compare this to an individual that is deconditioned or elderly, when they have a fall or set back it will significantly affect their quality of life as well as their ability to recover.
So we need to build the base!!
Raise the floor! -Craig Leibenson
This is again especially crucial for the populations described in the myth if you want to be ready and able for your children or grandchildren the best thing you can do is become more resilient, expand your foundational movement base, learn new tasks that challenge balance, strength, and readiness.
SCHEDULE NOW IN OFFICE OR FOR A TELEHEALTH SESSION TO DISCUSS YOUR LOW BACK PAIN
10. You will always have to do your back exercises
The exercises that you will be guided on will always be progressive.
Keep in mind a deadlift is a back exercise, so… we might encourage you to do deadlifts for the rest of your life.
Spoiler alert!! Deadlifts do not hurt your back! In fact, they make them stronger and better if done correctly.
So yes, in this case, you might always have to do your back exercises, but at the same time the previous exercises that were given in your acute phase or your building phase will eventually fade out as your progress.
Now I still do mine from time to time to check back in and look for any deficiencies or to brush up on some activation and foundational principles. Again getting good at the basics take you a long way.
What if instead of thinking I always need to do these so that I do not have pain, we rephrase it as I do these back exercises to continue to be strong!
Are we simply doing things to not suck or doing things to be better!
I would rather look forward than dwell on where I have been. Trust the process, do the basics well and allow your foundation to support you!
6 Truths About How To Stop Back Pain
1. Your back is strong
There are a number of different publications that dive deep into the exact amount of load tolerances the spine can withstand. And without going into specific numbers, we can still confidently state that our backs are crazy strong!
Now it must be said that some backs are stronger than others and why this is the case. But if you look to see what some humans are capable of whether it is feats of strength in competition or feats in strength unknowingly to save of life our bodies can do some amazing thing.
We have all seen on the amazing world wide web awesome pictures of individuals in their 80’s lifting crazy amounts of weights, and you think, what the hell? How can they do this? How is this not crippling them?
Strength is inherent in us due to our structural makeup, but it is also something that is developed. So although you might not feel it now, it is 100% possible to achieve it!
But it is more common that we will put a rate-limiting factor on our capabilities due to worry, frustration, or pain. Which I will add is completing natural and common.
Our role as a provider is to highlight a path that allows you to freely determine just how strong you are. The stronger you feel, the more strength you will exhibit, and low and behold, you body will start to adapt and become yet more resilient and robust.
All of a sudden you are in the amazing feed-forward loop of strength and resiliency.
But I understand in reading this if you are in pain you might not feel this way or imagine that this is a possibility, and that is why you need someone in your corner. If not yourself then let it be us!
We will show you the way to a better stronger life!
SCHEDULE NOW IN OFFICE OR FOR A TELEHEALTH SESSION TO DISCUSS YOUR LOW BACK PAIN
2. Movement will help
“Motion is lotion”
“Rest is rust”
There are a number of different phrases that hammer at this point that movement is key!
“If you are not moving then you are losing”
Why is it important?
Well, you see our bodies are very good at being efficient. And when it starts to realize that you are not moving enough, it oddly becomes better at not moving. And if you get better at not moving, well then you are pretty much stuck.
But if you start to move, then your body becomes better at moving, and the more you can move despite having a little bit of pain then your body will start to put the pieces together that:
“I am moving and I am moving with minimal pain”
“Then I must not be as beat up or hurt as I thought originally”
“I should try this other thing that hurt and see how it feels”
The movement investigation provides your body with a frame of reference to a map of the areas that are good to go and not good to go.
Your go no gos! Are simply put on the back burners
But everything else is fair game and now you can start to live your life again knowing and having a better understanding of you pain patterns and movement behaviors around your pain!
This is the most empowering thing for an individual in pain.
The fact that you can control if you are in pain or not based on what movements you do will simply speed up the recovery process and make you more resilient and empowered when it comes to pain management!
3. Sex can still be enjoyable
Due to the dynamic nature of the activity, many individuals struggling with lower back pain often will report the difficulty in connecting with their significant other. At first glance, especially if you have not experienced this type of pain to the level that would create this friction you might not have experienced how frustrating this would be on an individual and their relationship with their significant other.
How do we fix this to keep the spark alive!
Well, if you have made it this far you will gather that we will probably start by determining what movements or positions hurt and what feels better. World leader in spinal biomechanics, Dr. Stuart McGIll, has provided a reference list for individuals to use to better help them navigate what positions might prove to be more beneficial for individuals.
Having this knowledge will be extremely beneficial for you and your partner, as well as helping you continue on the path of recovery with reduces instances of flare-ups or pain bouts.
Understanding back pain can be very complex and what we know about it presents differently for everyone. But what we do know is that the old mentality is not servings us well and a new paradigm shift is happening, where people know they do not want to be reliant on medications and they definitely do not want to have surgery if they can do something about it. We have something you can do about it and trusting the process with a plan will be extremely rewarding to you.
This is not just about getting out of pain this is also about getting back your life. Being able to connect with your significant other has more benefits than nearly everything we have discussed. The relationships between your family and your friends will be strengthened.
Tracking process does not only mean less pain, sometimes it means we can do more with the same amount of discomfort or that it does not make it necessarily worse. So you if can apply this knowledge to do more activities that you enjoy with either the same amount of discomfort (more resiliency) or less discomfort (consistent improvement) then we are on the right path for recovery!
If you feel that your relationships are struggling as a result of the pain you have been experiencing please reach out to us today. We are able to provide you hope and benefit in the office or through telecommunications methods. We will find a way to help!
SCHEDULE NOW IN OFFICE OR FOR A TELEHEALTH SESSION TO DISCUSS YOUR LOW BACK PAIN
4. Let your body heal and it will
“Stop picking at it!”
We have all heard this at some point in our lives. Humans being the curious creatures that we are, seem to always be messing with our pain and picking at it.

Now that being said, we must understand that letting your body do what it needs to do does not mean sit around and wait.
Consider that much of your pain might be coming from compensation patterns or overly guarded muscles in the absence of tissue damage, especially if you had had pain for some period of time.
More importantly, we are referring to when we have a flare-up or acute pain we must map out the positions that are aggravating our symptoms. These movements, positions, activities, or behaviors are essentially just picking at the scab that is trying to heal itself. If you are able to modify these behaviors and movements temporarily you will allow the process to run its course. You can still move and be active we are just walking around a certain area for a certain period of time. As the sensitivity reduces then we introduce those back in with a systematic process that encourages self-advocacy and confidence!
More confidence = less pain = more movement = more confidence
We switch out of a negative feedback loop into a positive reinforcement loop.
Many of us will naturally do this, but we get stuck in the process of letting things “heal” and we do not progress. We fear to move and fear the slightest bit of pain thinking we are making things worse or not letting it heal.
Keep in mind that pain does not equal harm. Often this is simply and alarm system that triggers us to be cautious with whatever we are doing to prevent us from doing something more.
5. Auditing your lifestyle and what is important will help you understand how to stop back pain
This one might hit some of you a little harder.
Now when I say audit I simply mean taking a step back and gaining a better understanding of where you are, where you want to be, and what you are doing to get there. Sometimes we want certain things but we are not doing the right things to get there, or we are trying to make up and doing too much.
There are various different ways in which this could play out but hopefully, you can get a sense of what we are trying to go after here.
For instance, if you want to be healthy and have strong joints that go move well and not be painful, the Olympic lifts that you are doing in your fitness class might not be the best choice of movements to be performing. So when we say audit it comes down to many different factors.
Now for many of us, this statement is also true when we audit how much we are not moving throughout the day. Sedentarism is slowly rusting us away and aging us faster than our chronological age is. We are living longer and unhealthier.
So we integrate, we know there are things that might not be able to change 180 degrees in your life but if we can integrate some better habits for you back and your body you will start to feel more energized and not drained by your pain, your confidence will go up encouraging you to participate in more activities that you enjoy, and your overall lifestyle improves. Small consistent alterations can have a huge impact.
Breath | Move | Live
Ha, easier said than done right! You do not have to go at this alone ya know! We can help you create achievable, actionable steps so that this process is more streamlined ensuring your success.
6. Deadlifts are good for your back
We will finish with a bang here because for many of you out there you might have been told by a provider that you should ever deadlift lift that it is bad for you back, or you have been scared to perform anything like this because you suffered from a back pain episode following a deadlift movement.
Well, spoiler alert! You deadlifting or hip hinging every day to some capacity whether you are picking something off the ground, leaning forward and balancing, or unloading the dishwasher so this is important.
Now it must be said before we dive into the conversation that spinal flexion is normal and should be encouraged and performed. By preventing spinal flexion with everything that we do we are splinting one of the most important ranges of motion in our bodies that will be challenging to restore. When we encourage hip hinging/deadlifts we put it on a spectrum.
Certain movements will look similar to a hip hinge but have obvious spinal flexion, this might be something like picking up your keys off of the ground or petting the dog, low level of complexity and obvious low loading. On the other end of the spectrum is a heavy barbell deadlift that would require absolute perfect form and technique to reduce spinal flexion especially under load.
Everything else falls in the middle, which means we need to train on the left, to the far right, and in the middle. Creating a movement awareness model in your mind makes you more prepared for anything position, shape, or situation you are thrown into.
With that being said though, we will be encouraging weight hip hinging also known as deadlift! They are actually and arguably the best thing that you can be doing for you back!
Now if they hurt your back you are doing something wrong.
But!
If I can get you to deadlift a weight that is challenging for you or that you have not done before in the past and you can do it well without any pain we could probably argue that your back is ok and it is not broken. In fact, we could argue that your back is strong, and whatever doesn’t break us down will only make us stronger, and if you are stronger you can withstand more without getting hurt, and if you can withstand more without getting hurt you can do more and serve more and be more!
So all in all deadlifts save lives!!
But really this movement is one of the basic human movement patterns and strengthening it will encourage better movement patterns and strength that can be utilized when needed without any fear of getting hurt.
Conclusion
Hopefully, you were able to take away one piece of valuable information that will help you better learn how to stop back pain.
Our role is to help challenge you to create hope for the future and actionable steps for your success.
Invest in yourself and your future today right now. Wasting time only delays what you already know and that is change needs to happen. Take the first step to owning up to the pain and changing your future today!
There are many elements to back pain and in no way are we saying that it is as simple as we have laid out above for everyone. But I hope you have a little more confidence that what you are experiencing can be normal, and that there is a way to find comfort and conquer the pain that you are experiencing.
This article is intended to give you insight into the many elements of back pain while demonstrating the faults or myths around back pain and some encouraging points directed towards getting over back pain. If you have additional questions you can always reach me at 303-717-6323. We do not want anyone to be suffering and if there is anything that we can do to help or any value in which we can provide, we will do it!
So please reach out and let us help you get over this!!
Severe Non-Operative Disc Herniation Case Study
Severe Non-Operative Disc Herniation Case Study
The advancements in medical knowledge and interventions are at an all time high these days! Which is absolutely amazing and fantastic. But at the same time in this information age how do you ascertain what is the best route you should take for various medical conditions, illnesses, or injuries?
It depends.
I wish things were more black and white when it comes to medical intervention, and for some issues and conditions the lines are definitely a little more definitive. But for the most part everything is open to interpretation.
BUT!!! The most important thing to remember is that you have a say! It is your body and you need to advocate for yourself about what you feel comfortable and understand, so ask the questions!
You may find yourself asking right now, “Why is he yelling at me?”
No yelling just a strong emphasis to be speak up because I have a story to share with you about a patient that did speak up (figuratively) by asking questions and making a decision based on the facts.
What comes to mind when you hear the phrase, lumbar disc herniation?
Before and even partially during my training and postgraduate education even I thought:
- Extreme pain
- Leg weakness
- Numbness and burning pain
- Back surgery
You are not wrong if these thoughts come to mind, but keep it mind it is a gray area.
Does everyone who has a disc herniation experience these pain cycles or interventions? NO!
Do people have surgery without these symptoms? Sometimes.
Signs that you should seek orthopedic evaluations:
- Progressive neurological symptoms or worsening of symptoms. This is usually seen or described as the pain is traveling further down the leg and the intensity has been progressively getting worse.
- Progressive muscle weakness. Often times there is some minor motor weakness associated with disc herniations, if this progress further assessment and evaluations should be explored.
Lastly if you are experiencing any sign of what is known as cauda equina syndrome or saddle paresthesia or symptoms, please seek out immediate medical attention at your local urgent care or ER and let them know what is explicitly going on. This is no time for prudeness explain all the symptoms you may be having below the belt.
Jessica’s Story
Jessica was referred to our office for lower back pain that began just after she had given birth to her son Geoff. The pain was almost felt immediately after birth once the adrenaline and hormones leveled out. She was managing being a new mother well with nursing and the 1,000 other things that are involved, but her lower back pain was persistent and at times very painful.
Jessica’s pain was worse after prolonged sitting, and as a new mother picking up nursing for the first time with cluster feeds and all, you may find yourself sitting for some time. This pain began to progress and turn into some additional hip tightness and mild burning pain in the hip. Soon waking up in the morning began painfully and getting dressed and putting on socks and shoes turned into sweats and sandals.
After our detailed evaluation and exam, we believed that there was some degree of disc irritation present. Although we did not have an MRI to confirm we would treat it as such with our disc protocols and training the patient how to hinge at the hips properly and manage the loading of the lower back in addition to her postpartum rehab exercises to rebuild the core. Her progress and pain had been doing very well to the point where she decided to reduce the frequency of her home care and lost some of the training principles we discussed in regards to hinging and picking up the baby, etc.
Needless to say, Jessica’s pain started to return and was a little more aggressive this time around. One morning she was getting up off the ground with her son and started to feel some mild numbness and pain in the saddle region of her pelvis. (Think of the area of your body that would be touching a saddle when riding a horse, yeah this is a do take chances kind of area)
Jessica reached out to her PCP and was able to get in with an orthopedic doctor 2 days later, and then reached out to us after the appointment. They performed an immediate MRI that revealed a L5/S1 disc sequestration that was putting pressure on the nerves. They prescribed a steroid pack to help reduce the inflammation to prevent further pressure. Now a disc sequestration is when the disc completely opens as an opposed to just bulging out. This can actually cause more progressive symptoms but in some regard, this can actually start a quicker healing process compared to standard disc bulges.
** It must be stated that this is a scenario that immediately needs to be brought to an orthopedic surgeon attention**
While being managed by the orthopedic doctor Jessica was inquisitive and began asking as many questions as she could. Our discussions pointed out that there have been positive outcomes without doing surgery if symptoms do not progress and the that the body will eventually reabsorb the disc material that has been pushed from within the disc.
The orthopedic surgeon stated that if she would have come in a day earlier he would have recommended an emergency surgery based on her symptoms, but a day later Jessica came in and now indicating she wanted to wait to see if symptoms progress she is able to hold off on what would have been an “emergency surgery”.
Continuing to manage inflammation and reduce pressure on the disc with movement-based principles. Jessica’s symptoms slowly began to subside and reduce as time went on. Her saddle numbness was still present but pain was down, and slowly the radius of the numb area was dropping as well. One day Jessica reached out to us stated that all of her symptoms have returned back to normal.
This can be a very serious issue if not managed properly, evaluate and explore what you are feeling to give your provider the best insight as to what is going on and ask for alternative therapies if that is something that you are interested in. There are times when symptoms include the listed provided above as well as other progressive symptoms that involve bowel and bladder symptoms where one should NOT wait to seek medical attention.
Conclusion
The take-home message here is there are multiple roads to Rome. Often times the recommended intervention might be too invasive or extensive for what you were hoping to do, so explore your options and ask your providers questions. In this case, the patient was fortunate enough to not have her symptoms progress and she was able to rehab and get back to leading an active life with her toddler without going through surgery for an extensive disc herniation or sequestration.
This again is one of the more extreme cases to show one end of the spectrum, if you are diagnosed with a disc herniation or bulge and you might have symptoms that are down your leg without progressive motor loss or progressive neurological conditions you are most likely able to return and rehab without undergoing any surgery.
If you are unsure whether or not you are in a position to continue down more conservative options and/or you are concerned about going down more invasive protocols please reach out to us and we would be happy to discuss your options!
Do You Need X-rays to See a Chiropractor?
Do You Need X-rays to See a Chiropractor?
X-rays are common practice for many practitioners in the chiropractic profession.
It is an amazing service that can help catch diseases and pathologies, it can be very helpful when looking for fractures, and it is fairly cost-effective for most situations.
But when does it begin to become an issue when everyone and their mothers are being put under X-rays when they go to the chiropractor?
We are going to be making this article very brief and to the point.
X-rays can be beneficial when necessary. Your providers that you are going to, that are relying on X-rays to treat you, are making you pay for unnecessary costs that will most likely not help your pain.
The American Chiropractic Association Has 5 Recommendations:
- In the absence of red flags, do not obtain spinal imaging (X-rays) for patients with acute low-back pain during the six weeks after the onset of pain.
- Do not perform repeat spinal imaging to monitor patients’ progress.
- Avoid prolonged or ongoing use of passive or palliative physical therapy treatments (such as heat, cold, electrical stimulation and ultrasound) for low-back pain unless they support the goal(s) of an active treatment plan.
- Do not provide long-term pain management without psychosocial screening or assessment for possible related psychological disorders, most notably depression and anxiety.
- Do not prescribe lumbar supports or braces for the long-term treatment or prevention of low-back pain.
How X-Rays Are Typically Used by Your Providers:
- X-rays to determine where to adjust
- X-rays used to scare people into prolonged treatment plans
- X-rays to monitor progress through the awfully long plans
- X-rays used to determine if the treatment plan got results
- X-rays used for additional ammunition to continue care if we did not see changes we wanted
Here are some fleeting thoughts for you all…
If your chiropractor needs X-rays to determine where to adjust, how do they know where to touch you if they are relying on the image to see where to go?
Perhaps putting your trust and investing your time, money, and efforts will be better spent on methods that will not rob you of your power and health!
Our skilled providers can easily manage and evaluate where to provide intervention without the need for X-rays and you typically get better results faster. Our focus is on you not what some snapshot image says about you.
Keep up the great work and LIVE LOUD!
Share with a friend or loved one.
5 Reasons Your Feet Hate You
5 Reasons Your Feet Hate You
It is sometimes crazy to think about your feet. I mean it is one of those body parts that just seem to be there. But when you consider that we are bipedal animals they basically do everything for us.
So here are a few reasons they are not too jazzed with how you have been treating them lately or for your whole life.
5 Reasons Your Feet Are Mad At You
1. You Never Give Them a Hug
When was the last time you touched your feet? I mean like grabbed that beauty pulled it in and gave it a nice squeeze. I bet the majority of you don’t even wash your feet all that well.
Ah, they are so far away.
We tend to forget that when we think about something our focus because more direct and intentional about those things and then it starts taking off from there. You start to realize that you have some sore points on the bottom, or a weird nail thing going on that you didn’t even notice before.
Now the point is not to focus on weird feet things that you may or may not have but more importantly, we are trying to get you to understand that your feet are a very important part of your body especially as it pertains to movement, health, and fitness.
2. You Force Them To Take Odd Shapes
I know we all know this but we basically turn a blind eye, and men and women are just as guilty to blame because some of the guy’s shoes out there that I have seen are crazy.
If your shoe comes to a point then your toes are pointing to you the middle finger!
We are not just talking about the front of the shoe we are also throwing in their heels, width, arches, all of it!
Now stop freaking out, cause I know ½ of you right now are thinking, “well I have flat feet” or “my arches are too high and they need support”.
This is not a one shoe size fits all conversation! (hey ooooo)
But one might argue that your feet are now this way because of what you did to them in the past. Neither here nor there we are trying to progress forward and not reminisce too hard on the past and what we could have done differently.
BUT!!!
All we are saying is that if you try to put a soft peg in a hard square hole eventually that peg will change its shape to fit in the constraints in which you are forcing it in.
Ideally, you want to have enough space in your foot wear for your foot to mold and adapt and change based on the various tasks and demands you are putting it through. Something as simple as walking required the middle part of the foot to splay out and spread to help disperse forces, all while transitioning from various positions of supination and pronation.
All of the micro-movements, although mostly unconscious mostly because we are disconnected from our feet see bullet #1, control lower limb positioning above, hip function and movement, pelvic alignment, and so on and so forth.
3. They Never Get a Massage
We could really argue this for our whole bodies. Most of us do not give ourselves the TLC that we deserve.
But with the shoes, you wear, walking throughout the day, sports and activities we do, the feet take a good beating!
Something as simple as taking a tennis ball, lacrosse ball, spikey ball, edge of a coffee table, really whatever you want and pushing and poking and digging in can create a massage session for your feet. This can reduce tight muscles and tension throughout the feet.
It will also improve joint mobility and motion which is absolutely critical for overall function of the feet.
Not to mention all of the benefits in proprioception you get afterward. Just touching an area of your body brings more awareness to the area, more awareness creates better mind to body connection which is what proprioception essentially is. The more aware I can be the better I can manage and operate that area of my body.
4. You Suffocate Them
I am very surprised by how many people I work with who report wearing their shoes for literally 95% of the day.
They wake up and spend maybe 30 min to an hour barefoot or in socks and then throw shoes on and do not take them off until they are getting ready for bed.
Let those puppies breath!!!
Have you ever tried to do a squat or bend down towards the ground in a new pair or jean or some kind of tight clothing? Your hips and knees cannot bend and move and they should and thus your ability to move is altered and changed.
The same is true for your feet in your shoes. If they do not have the simple spacial capacity to move when we are weight-bearing then the joints will not be able to move and ultimately start giving you issues. On the performance side, we need the toes to be bending and spreading out to ground us and distribute force adequately among the whole foot.
The better the distribution the more balance we have and more balance equal more control and we could argue that better control can lead to efficiency and performance.
5. They Don’t Live To Their Full Potential
As with most of our joints, our feet do not live up to their full potential.
What do we mean by this?
We use them in a very limited capacity and they are not able to do what they have the ability to do. Even if we are considering wearing shoes in which the feet are somewhat limited, depending on the type of shoe, we are not doing things barefoot.
So what do we suggest.
Find times and opportunities especially around the house or your yard to start wearing your shoes less and play and move with your dogs or your kids to challenge your feet, to make them stronger, to mobilize them and keep all of your joint healthy.
As we have stated many times in our articles motion is lotion, the more mobile and free we can keep our joints the healthier they will be, the better they will perform, and they will feel amazing!
So kick off those shoes and live a little!!
Top 5 Exercises to Relieve Mid Back Pain During Pregnancy
Top 5 Exercises to Relieve Mid Back Pain During Pregnancy
Do you have back pain postpartum? If your answer is yes, you’re not alone.
I’m Dr. Nichelle Gurule with Live Loud Chiropractic and coaching out of Lafayette, Colorado. I have patients asking me all the time how they can relieve their neck and mid back pain that they have after having a baby. We’re going to go over the top five exercises that you can do to help with postpartum mid back pain. A lot of the time it stems from the postpartum habits that create posture that is less than ideal. It is important to recognize we want to work on a mix of spinal mobility, stretching, and strengthening. The top five exercises we’re going to go over to help with postpartum upper back pain are banded As, double chins, thread the needles, thoracic foam rock out, and a pec stretch.
PLAY VIDEO ⬇︎
What Causes Back Pain Postpartum?
You suddenly go from doing whatever you’re doing, to taking care of an infant 24/7, which mostly means holding them, staring lovingly at them, feeding them, whether it’s bottle feeding or breastfeeding), and just holding them while they’re sleeping.
- We’ve created a “new mom posture” that is commonly rounded with your head looking down at your baby. Our neck muscles are struggling. Our mid back muscles are weak and lengthened. Our pecs are tight and shortened. And our mid back is rounded in this flex posture all the time.
- We have a core that is not as strong; it’s weakened as those muscles get lengthened through the course of pregnancy. And some women will have a remaining diastasis (a separation of their abdominal wall) postpartum. Their core is not as strong, especially in the abdominal region. It’s easier just to slouch.
- Fatigue plays a big role. We’re tired! Relaxin is still elevated for up to five months postpartum, and up to a couple months after breastfeeding.
- Hormones cause laxity of the connective tissue.
- We’re not moving as much anymore. So we are slouched, taking care of baby and not getting in that movement because we are trying to allow our bodies to heal.
Top 5 Exercises For Mid Back Pain Postpartum
So a combination of all that leads to posture that’s little less than ideal. What we want to do is stretch out our pecs, because if they’re tight, they’re going to pull us down. We want to strengthen the mid back and neck muscles, gain mobility in the mid back, get into extension and out of flexion. Let’s dive into all of this with our top five postpartum exercises for relieving mid back pain.
1. Banded A’s.
Banded A’s will help strengthen the mid back postpartum. Think about activating your lats and pulling your shoulder blades down and back. Come into an athletic stance, and slow and controlled, bring the band out into an ‘A’ position. I like the pace of five seconds out, five seconds returning. You can wrap the band around a kitchen table leg, a desk leg, or even a banister.
2. Double Chins
Double chin helps strengthen the neck. Interlace your fingers and place them behind your head. Then push your head directly back into your hands. You can do 10 reps where you hold for one to two seconds; or you can just hold for 20 to 30 seconds. You can do it without interlacing your hands, there just won’t be as much of a force to press into. You can press into a headrest in the car, or if you’re feeding your baby and you’re against a wall, you can press your head against the wall. But be aware that it’s not tucking the chin, it’s bringing it directly back.
3. Thread the Needle.
Thread the needle is great for getting the thoracic spine mobility that gets restricted during a lot of those new mom postures that we have with baby. To start, come down on the ground in a table-top pose. Place your hand behind your neck, then drive your elbow up toward the ceiling, then interlace it through. Try to get as much range of motion as you can in this rotation.
4. Thoracic Spine Roll Out
If you have a foam roller, the thoracic foam roll out is great for getting more mobility and extension of the thoracic spine that’s been flexed so much. Start at the bottom of your thoracic spine, which is where your your ribs end. Either cross your arms over your chest, or have them up overhead. Then rock and pivot over without lifting your hips. Then roll it up a little bit and repeat this motion. Once you get up to the top of your back, you can then open up your arms, relax your head, and stretch out your pecs.
5. Couch Stretch
The couch stretch works on an extension of the thoracic spine that’s been in a lot of flexion during the postpartum early days. Open up your arms nice and wide on the couch, and then drop your chest through. You’ll get that extension in the mid back, and the pecs will get stretched stretched at the same time. You can also do a pec stretch in a doorway or against the wall.
Conclusion
So those are the top five exercises that you can start now to help work on that mid back pain that you’re having postpartum. Other than things that you can do at home, I recommend chiropractic care, rehab like some of the movements I just gave you, massage, and acupuncture. And then finally, put heat on the area. Sometimes relaxing those muscles with a hot bath or heating pad can be really helpful to relieving that mid back pain you’re having postpartum.
Keep up the great work and LIVE LOUD!
Share below with a friend or loved one.
What is Sciatic Nerve or Sciatica Pain?
What is Sciatic Nerve or Sciatica Pain?
Everyone has an Uncle Frank! You know Uncle Frank, the uncle who when you politely ask, how have things been going, responds with: “OOOOH my sciatica has been acting up again.” As if it was a chihuahua that has been getting into the trash to dig out a taco bell bag and they cannot figure out why it would be doing such a thing.
But just like Uncle Frank, most people are somewhat confused when it comes to the term sciatica and what it actually means or what the symptoms actually are.
So we will run through and give you everything you need to know about sciatica and what you may be able to do if you think you may have it.
What is Sciatica?
When someone refers to their sciatica acting up they are really referring to their sciatic nerve. To simply say my sciatica is acting up is no different than saying my back is acting up. Well is it your upper back? Your lower back? You get the point. They are simply stating a known buzzword or phrase that has little to no context.
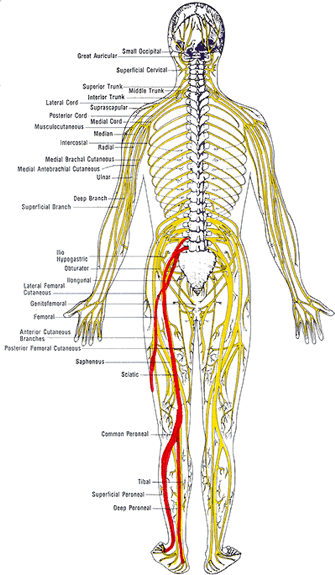
The sciatic nerve is one of the largest nerves in your body that is comprised of a number of lumbar and sacral nerve roots that exit the spine and combine into one larger nerve. When evaluating the image of the nerve we can see how the different levels of the spinal nerve roots blend together to form the sciatic nerve. This is important to understand as we will highlight how this helps determine the origin of irritation or pain for someone who is dealing with these symptoms.
The sciatic nerve then travels along the pelvis on each side and will begin to branch off into various different nerves that supply motor and sensory function to the lower extremity or legs. This too is also very critical information that will provide a great clinician detailed information about what and where there might be an underlying cause to your pain, numbness, or weakness.
As the nerve continues from the pelvis it runs along the back of the legs following the hamstring muscles to the back of the knee. What if tight hamstring muscles are really a result of a tight nerve? This may create valid arguments as to why tight hamstrings are not necessarily the cause of lower back pain but a response to the pain and a generator of guarding and protection.
A brief comment on the anatomy of nerves. Nerves like any other tissue structure in the body are compromised of cells and these cells require nutrients and oxygen just the same. And the also respond the same when their blood supply is occluded or compressed. Interesting enough because their operational functions are critical for many different functions throughout the body, it does not respond well when they are irritated.
In our office, we commonly portray the picture of the irritated friend, who that would otherwise be cool when planks are played on him now will all of the sudden lash out and overreact because he was already irritated. These normal stimuli that would not evoke a response have now set off a cascade of furry and fire! Internally our nerves are operating at a very similar capacity. If they are irritated through a chemical response, physical compression, or too much tension any simple act such as even putting on your socks and shoes can create an inflated pain response.
This concept is absolutely critical when trying to tease out the correct responses one should be trying to imply in order to seek recovery and reduce their overall pain sensitivity. Because the more you are in pain, the more pain you will be in.
While there are still some minor differences in opinion as to the the true definition of sciatica or sciatic pain there are some publications that have done the work for us to include some of the inclusion criteria for classifying sciatica. In the article “Clinical diagnostic model for sciatica developed in primary care patients with low back-related leg pain” in PLOS ONE 2018 authors have provided us a clear scoring table to predict the probability of sciatica. Reported symptoms in the studies were: reported pins and needles or numbness in the involved lower limb, reported pain below the knee, leg pain that is worse than their back, they had a positive straight leg raise test and/or femoral nerve test and/or slump test, and did they have any myotome (muscle) / reflex or sensory deficits in the lower extremity.
Based on the sum score as seen in the table in the article HERE one could then determine the probability of having sciatica.
This does not indicate the exact cause of the pain though it simply classifies where the pain is, although we may have some insight as to what the driving cause is from the history and intake questionnaires.
Based on who your provider is and their background will always have a slightly biased direction as to what they believe the underlying cause is, and that is why a full examination and provocative testing is best done to complete the evaluation and determine the best course of action. Based on the above symptoms you can see that some individuals can present with different types of symptoms and different locations of symptoms making this somewhat of a challenging issue.
More importantly than anything it continuing to have a conversation with you the patient to determine what were some of the activities we were or were not doing at the time the pain had come on. This may provide your clinician with valuable information as that what you should be doing and potentially not be doing. This also bridges us into what you want to be doing.
More often than not the fix or relief for these symptoms is found in the directional preferences of movement and the short term avoidance of others.
For example: Let’s say Uncle Frank’s lower back was sore from shoveling snow from a recent snowstorm. It was a heavy storm and he was hunched over for a period of time and now he struggles to put on his boots, socks, and pants. When he flexes forward he aggravates the nerve roots that were pissed off from the shoveling and now he is in more pain. But through guided movement therapies, we help Uncle Frank learn how to hip hinge more appropriately and reduce excess loading in the lumbar spine and improve the shared loading into the hips, all of the sudden what appears to be the exact same movement had reduced the patient’s discomfort and allowed them to improve their function. So the directional preference, in this case, was avoiding flexion of the spine when bending forward. This overtime will eventually not be the case but while things are sensitized it is wise to follow these preferences to help reduce pain and allow for faster recovery.
Let’s review the main way nerves get pissed off or irritated and cause us pain:
- Compression
- Tension
- Chemical
There are other pathological reasons for nerve irritation but we are focused primarily on functional and biomechanical alterations that would create your symptoms.
You will not always know that you have an irritated nerve though as many of the symptoms are different and occur in different areas for individuals. Here is a list of common symptoms:
– Radiating pain down the arm or the leg
– Muscle guarding, spasm, or cramping
– Numbness
– Pins & needles
– Aches that do not ease with pain medication
– Difficulty finding a comfortable, pain-free position
– Latent pain/tightness in response to stretching, posture, or activity, and
– No pain, but a tightness that does not loosen up (e.g. in the neck, back, hamstrings, etc.)
In our case for the sciatic nerve, you will see these symptoms occurring as high in the hip or glute/butt muscles and down all the way into the toes.
What to do if you have an irritated nerve?
Try not to piss it off more!
Easier said than done right? It is really about paying more attention to when you have symptoms and what was done prior. For some, it might be that you were literally not doing anything. Sitting and not moving might be aggravating depending on how much tension or compression is in the nerve. This is why it is important to have a proper evaluation and consultation with a professional.
With the sciatic nerve one of the most common complaints, is either a tight hamstrings or tight calf muscles and this prompts individuals to throw a leg up or start stretching these areas to only irritate things further. If it is a lumbar root driver, then prolong sitting or driving will commonly aggravate the symptoms.
How we work through this pain in our office:
- Directional Preferences
- Hip Hinges and Spinal Hygiene
- Passive Lumbar extension (McKenzie Extensions)
- Neural Mobilizations
- Lifting Weights and Resistance Training
- Directional Preferences
As mentioned above you want to understand and determine what directions are not responding well to the patient and find the positions that offer relief and or reduce symptoms. Progress is not always zero pain but also simply reduce symptoms or less pain down the leg. When the pain is relieved through these directional preferences we are taking either compression off of the nerve allowing it to reperfuse with blood and reduce chemical irritation, relieving compression forces and reduce signal transmission, or putting slack in the line reducing irritation. And the more you can offer this to the nerves the better they will respond.
1. Hip Hinging and Spinal Hygiene
Being able to hip hinge will have great carry over to any and most aspects of life as it affords you the ability to carry out functional tasks most efficiently as you learn to balance the load between the low back and the hips. When we can hip hinge the glute and hamstring are more involved reducing the amount of tension also put through the passive structure and nerves. This will also relieve any excess tension or pressure that might be pushing through the discs and causing nerve root irritation
2. Passive Lumbar extension
Many times the directional preference that responses best for individuals with sciatic nerve pain is the extension of the lower back. This is from McKenzie’s work and the active care model approach of self-managing your pain. These can be performed as press up or hip drop, but the key is to keep the low back muscles and butt muscles passive and relax. This will help reduce lumbar disc bulges and herniations, as well as put slack in the nerve roots, and give the guarded muscles and opportunity to relax. This tool is so powerful it is often overlooked. It is also recommended to be used throughout the day to relieve tension or tightness from prolong sitting.
3. Neural Mobilizations
Neural mobilizations are also referred to as nerve glides or nerve flossing. The intention is to keep the nerves mobile and sliding through the sheaths that surround them. Connective tissue restrictions can create kinks or binding restrictions that pull on the nerve creating more irritation. This may also be a result of inflammation accumulation from an injury that we want to try and maintain neural mobility. These should be done under the guidance and instruction of a professional as it is easy to put too much tension in the nerve and aggravate it further.
4. Lifting Weights and Resistance Training
We want to try and maintain as much of our functional capacity as we can through this time and there is no other best way than adding some resistance training. Resistance training will stimulate the body to continue adapting and recovering. It helps solidify technique and form. Most importantly if provides contextual feedback for how the body is feeling in real-time. If you are able to perform, lift, or do as a task without discomfort or pain then your body and nervous system will start to put together the pieces that your body is doing well and that you are not falling victim to these symptoms. The less you are in pain the less you will be in pain and if you can do that with challenging tasks then even more power to you!
Conclusion
The intention of this article was to provide insight and guidance into the most common causes of sciatic nerve pain or “sciatica”. This was in no way intended to diagnose your symptoms and what is causing the pain. There are other opportunities that may create similar symptoms and it is always suggested that you schedule a consultation and evaluation with a professional.
I’m Dr. Antonio with Live Loud Chiropractic and Coaching in Lafayette, Colorado. If you have any questions I am more than happy to help answer what I can and you can always call my cell phone number. 303-520-8974