What is Sciatic Nerve or Sciatica Pain?
Everyone has an Uncle Frank! You know Uncle Frank, the uncle who when you politely ask, how have things been going, responds with: “OOOOH my sciatica has been acting up again.” As if it was a chihuahua that has been getting into the trash to dig out a taco bell bag and they cannot figure out why it would be doing such a thing.
But just like Uncle Frank, most people are somewhat confused when it comes to the term sciatica and what it actually means or what the symptoms actually are.
So we will run through and give you everything you need to know about sciatica and what you may be able to do if you think you may have it.
What is Sciatica?
When someone refers to their sciatica acting up they are really referring to their sciatic nerve. To simply say my sciatica is acting up is no different than saying my back is acting up. Well is it your upper back? Your lower back? You get the point. They are simply stating a known buzzword or phrase that has little to no context.
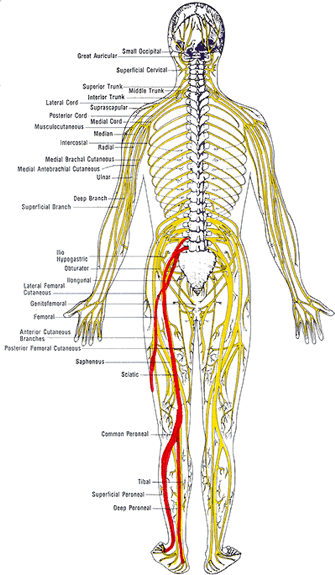
The sciatic nerve is one of the largest nerves in your body that is comprised of a number of lumbar and sacral nerve roots that exit the spine and combine into one larger nerve. When evaluating the image of the nerve we can see how the different levels of the spinal nerve roots blend together to form the sciatic nerve. This is important to understand as we will highlight how this helps determine the origin of irritation or pain for someone who is dealing with these symptoms.
The sciatic nerve then travels along the pelvis on each side and will begin to branch off into various different nerves that supply motor and sensory function to the lower extremity or legs. This too is also very critical information that will provide a great clinician detailed information about what and where there might be an underlying cause to your pain, numbness, or weakness.
As the nerve continues from the pelvis it runs along the back of the legs following the hamstring muscles to the back of the knee. What if tight hamstring muscles are really a result of a tight nerve? This may create valid arguments as to why tight hamstrings are not necessarily the cause of lower back pain but a response to the pain and a generator of guarding and protection.
A brief comment on the anatomy of nerves. Nerves like any other tissue structure in the body are compromised of cells and these cells require nutrients and oxygen just the same. And the also respond the same when their blood supply is occluded or compressed. Interesting enough because their operational functions are critical for many different functions throughout the body, it does not respond well when they are irritated.
In our office, we commonly portray the picture of the irritated friend, who that would otherwise be cool when planks are played on him now will all of the sudden lash out and overreact because he was already irritated. These normal stimuli that would not evoke a response have now set off a cascade of furry and fire! Internally our nerves are operating at a very similar capacity. If they are irritated through a chemical response, physical compression, or too much tension any simple act such as even putting on your socks and shoes can create an inflated pain response.
This concept is absolutely critical when trying to tease out the correct responses one should be trying to imply in order to seek recovery and reduce their overall pain sensitivity. Because the more you are in pain, the more pain you will be in.
While there are still some minor differences in opinion as to the the true definition of sciatica or sciatic pain there are some publications that have done the work for us to include some of the inclusion criteria for classifying sciatica. In the article “Clinical diagnostic model for sciatica developed in primary care patients with low back-related leg pain” in PLOS ONE 2018 authors have provided us a clear scoring table to predict the probability of sciatica. Reported symptoms in the studies were: reported pins and needles or numbness in the involved lower limb, reported pain below the knee, leg pain that is worse than their back, they had a positive straight leg raise test and/or femoral nerve test and/or slump test, and did they have any myotome (muscle) / reflex or sensory deficits in the lower extremity.
Based on the sum score as seen in the table in the article HERE one could then determine the probability of having sciatica.
This does not indicate the exact cause of the pain though it simply classifies where the pain is, although we may have some insight as to what the driving cause is from the history and intake questionnaires.
Based on who your provider is and their background will always have a slightly biased direction as to what they believe the underlying cause is, and that is why a full examination and provocative testing is best done to complete the evaluation and determine the best course of action. Based on the above symptoms you can see that some individuals can present with different types of symptoms and different locations of symptoms making this somewhat of a challenging issue.
More importantly than anything it continuing to have a conversation with you the patient to determine what were some of the activities we were or were not doing at the time the pain had come on. This may provide your clinician with valuable information as that what you should be doing and potentially not be doing. This also bridges us into what you want to be doing.
More often than not the fix or relief for these symptoms is found in the directional preferences of movement and the short term avoidance of others.
For example: Let’s say Uncle Frank’s lower back was sore from shoveling snow from a recent snowstorm. It was a heavy storm and he was hunched over for a period of time and now he struggles to put on his boots, socks, and pants. When he flexes forward he aggravates the nerve roots that were pissed off from the shoveling and now he is in more pain. But through guided movement therapies, we help Uncle Frank learn how to hip hinge more appropriately and reduce excess loading in the lumbar spine and improve the shared loading into the hips, all of the sudden what appears to be the exact same movement had reduced the patient’s discomfort and allowed them to improve their function. So the directional preference, in this case, was avoiding flexion of the spine when bending forward. This overtime will eventually not be the case but while things are sensitized it is wise to follow these preferences to help reduce pain and allow for faster recovery.
Let’s review the main way nerves get pissed off or irritated and cause us pain:
- Compression
- Tension
- Chemical
There are other pathological reasons for nerve irritation but we are focused primarily on functional and biomechanical alterations that would create your symptoms.
You will not always know that you have an irritated nerve though as many of the symptoms are different and occur in different areas for individuals. Here is a list of common symptoms:
– Radiating pain down the arm or the leg
– Muscle guarding, spasm, or cramping
– Numbness
– Pins & needles
– Aches that do not ease with pain medication
– Difficulty finding a comfortable, pain-free position
– Latent pain/tightness in response to stretching, posture, or activity, and
– No pain, but a tightness that does not loosen up (e.g. in the neck, back, hamstrings, etc.)
In our case for the sciatic nerve, you will see these symptoms occurring as high in the hip or glute/butt muscles and down all the way into the toes.
What to do if you have an irritated nerve?
Try not to piss it off more!
Easier said than done right? It is really about paying more attention to when you have symptoms and what was done prior. For some, it might be that you were literally not doing anything. Sitting and not moving might be aggravating depending on how much tension or compression is in the nerve. This is why it is important to have a proper evaluation and consultation with a professional.
With the sciatic nerve one of the most common complaints, is either a tight hamstrings or tight calf muscles and this prompts individuals to throw a leg up or start stretching these areas to only irritate things further. If it is a lumbar root driver, then prolong sitting or driving will commonly aggravate the symptoms.
How we work through this pain in our office:
- Directional Preferences
- Hip Hinges and Spinal Hygiene
- Passive Lumbar extension (McKenzie Extensions)
- Neural Mobilizations
- Lifting Weights and Resistance Training
- Directional Preferences
As mentioned above you want to understand and determine what directions are not responding well to the patient and find the positions that offer relief and or reduce symptoms. Progress is not always zero pain but also simply reduce symptoms or less pain down the leg. When the pain is relieved through these directional preferences we are taking either compression off of the nerve allowing it to reperfuse with blood and reduce chemical irritation, relieving compression forces and reduce signal transmission, or putting slack in the line reducing irritation. And the more you can offer this to the nerves the better they will respond.
1. Hip Hinging and Spinal Hygiene
Being able to hip hinge will have great carry over to any and most aspects of life as it affords you the ability to carry out functional tasks most efficiently as you learn to balance the load between the low back and the hips. When we can hip hinge the glute and hamstring are more involved reducing the amount of tension also put through the passive structure and nerves. This will also relieve any excess tension or pressure that might be pushing through the discs and causing nerve root irritation
2. Passive Lumbar extension
Many times the directional preference that responses best for individuals with sciatic nerve pain is the extension of the lower back. This is from McKenzie’s work and the active care model approach of self-managing your pain. These can be performed as press up or hip drop, but the key is to keep the low back muscles and butt muscles passive and relax. This will help reduce lumbar disc bulges and herniations, as well as put slack in the nerve roots, and give the guarded muscles and opportunity to relax. This tool is so powerful it is often overlooked. It is also recommended to be used throughout the day to relieve tension or tightness from prolong sitting.
3. Neural Mobilizations
Neural mobilizations are also referred to as nerve glides or nerve flossing. The intention is to keep the nerves mobile and sliding through the sheaths that surround them. Connective tissue restrictions can create kinks or binding restrictions that pull on the nerve creating more irritation. This may also be a result of inflammation accumulation from an injury that we want to try and maintain neural mobility. These should be done under the guidance and instruction of a professional as it is easy to put too much tension in the nerve and aggravate it further.
4. Lifting Weights and Resistance Training
We want to try and maintain as much of our functional capacity as we can through this time and there is no other best way than adding some resistance training. Resistance training will stimulate the body to continue adapting and recovering. It helps solidify technique and form. Most importantly if provides contextual feedback for how the body is feeling in real-time. If you are able to perform, lift, or do as a task without discomfort or pain then your body and nervous system will start to put together the pieces that your body is doing well and that you are not falling victim to these symptoms. The less you are in pain the less you will be in pain and if you can do that with challenging tasks then even more power to you!
Conclusion
The intention of this article was to provide insight and guidance into the most common causes of sciatic nerve pain or “sciatica”. This was in no way intended to diagnose your symptoms and what is causing the pain. There are other opportunities that may create similar symptoms and it is always suggested that you schedule a consultation and evaluation with a professional.
I’m Dr. Antonio with Live Loud Chiropractic and Coaching in Lafayette, Colorado. If you have any questions I am more than happy to help answer what I can and you can always call my cell phone number. 303-520-8974