Health & Wellness
Severe Non-Operative Disc Herniation Case Study
Severe Non-Operative Disc Herniation Case Study
The advancements in medical knowledge and interventions are at an all time high these days! Which is absolutely amazing and fantastic. But at the same time in this information age how do you ascertain what is the best route you should take for various medical conditions, illnesses, or injuries?
It depends.
I wish things were more black and white when it comes to medical intervention, and for some issues and conditions the lines are definitely a little more definitive. But for the most part everything is open to interpretation.
BUT!!! The most important thing to remember is that you have a say! It is your body and you need to advocate for yourself about what you feel comfortable and understand, so ask the questions!
You may find yourself asking right now, “Why is he yelling at me?”
No yelling just a strong emphasis to be speak up because I have a story to share with you about a patient that did speak up (figuratively) by asking questions and making a decision based on the facts.
What comes to mind when you hear the phrase, lumbar disc herniation?
Before and even partially during my training and postgraduate education even I thought:
- Extreme pain
- Leg weakness
- Numbness and burning pain
- Back surgery
You are not wrong if these thoughts come to mind, but keep it mind it is a gray area.
Does everyone who has a disc herniation experience these pain cycles or interventions? NO!
Do people have surgery without these symptoms? Sometimes.
Signs that you should seek orthopedic evaluations:
- Progressive neurological symptoms or worsening of symptoms. This is usually seen or described as the pain is traveling further down the leg and the intensity has been progressively getting worse.
- Progressive muscle weakness. Often times there is some minor motor weakness associated with disc herniations, if this progress further assessment and evaluations should be explored.
Lastly if you are experiencing any sign of what is known as cauda equina syndrome or saddle paresthesia or symptoms, please seek out immediate medical attention at your local urgent care or ER and let them know what is explicitly going on. This is no time for prudeness explain all the symptoms you may be having below the belt.
Jessica’s Story
Jessica was referred to our office for lower back pain that began just after she had given birth to her son Geoff. The pain was almost felt immediately after birth once the adrenaline and hormones leveled out. She was managing being a new mother well with nursing and the 1,000 other things that are involved, but her lower back pain was persistent and at times very painful.
Jessica’s pain was worse after prolonged sitting, and as a new mother picking up nursing for the first time with cluster feeds and all, you may find yourself sitting for some time. This pain began to progress and turn into some additional hip tightness and mild burning pain in the hip. Soon waking up in the morning began painfully and getting dressed and putting on socks and shoes turned into sweats and sandals.
After our detailed evaluation and exam, we believed that there was some degree of disc irritation present. Although we did not have an MRI to confirm we would treat it as such with our disc protocols and training the patient how to hinge at the hips properly and manage the loading of the lower back in addition to her postpartum rehab exercises to rebuild the core. Her progress and pain had been doing very well to the point where she decided to reduce the frequency of her home care and lost some of the training principles we discussed in regards to hinging and picking up the baby, etc.
Needless to say, Jessica’s pain started to return and was a little more aggressive this time around. One morning she was getting up off the ground with her son and started to feel some mild numbness and pain in the saddle region of her pelvis. (Think of the area of your body that would be touching a saddle when riding a horse, yeah this is a do take chances kind of area)
Jessica reached out to her PCP and was able to get in with an orthopedic doctor 2 days later, and then reached out to us after the appointment. They performed an immediate MRI that revealed a L5/S1 disc sequestration that was putting pressure on the nerves. They prescribed a steroid pack to help reduce the inflammation to prevent further pressure. Now a disc sequestration is when the disc completely opens as an opposed to just bulging out. This can actually cause more progressive symptoms but in some regard, this can actually start a quicker healing process compared to standard disc bulges.
** It must be stated that this is a scenario that immediately needs to be brought to an orthopedic surgeon attention**
While being managed by the orthopedic doctor Jessica was inquisitive and began asking as many questions as she could. Our discussions pointed out that there have been positive outcomes without doing surgery if symptoms do not progress and the that the body will eventually reabsorb the disc material that has been pushed from within the disc.
The orthopedic surgeon stated that if she would have come in a day earlier he would have recommended an emergency surgery based on her symptoms, but a day later Jessica came in and now indicating she wanted to wait to see if symptoms progress she is able to hold off on what would have been an “emergency surgery”.
Continuing to manage inflammation and reduce pressure on the disc with movement-based principles. Jessica’s symptoms slowly began to subside and reduce as time went on. Her saddle numbness was still present but pain was down, and slowly the radius of the numb area was dropping as well. One day Jessica reached out to us stated that all of her symptoms have returned back to normal.
This can be a very serious issue if not managed properly, evaluate and explore what you are feeling to give your provider the best insight as to what is going on and ask for alternative therapies if that is something that you are interested in. There are times when symptoms include the listed provided above as well as other progressive symptoms that involve bowel and bladder symptoms where one should NOT wait to seek medical attention.
Conclusion
The take-home message here is there are multiple roads to Rome. Often times the recommended intervention might be too invasive or extensive for what you were hoping to do, so explore your options and ask your providers questions. In this case, the patient was fortunate enough to not have her symptoms progress and she was able to rehab and get back to leading an active life with her toddler without going through surgery for an extensive disc herniation or sequestration.
This again is one of the more extreme cases to show one end of the spectrum, if you are diagnosed with a disc herniation or bulge and you might have symptoms that are down your leg without progressive motor loss or progressive neurological conditions you are most likely able to return and rehab without undergoing any surgery.
If you are unsure whether or not you are in a position to continue down more conservative options and/or you are concerned about going down more invasive protocols please reach out to us and we would be happy to discuss your options!
Do You Need X-rays to See a Chiropractor?
Do You Need X-rays to See a Chiropractor?
X-rays are common practice for many practitioners in the chiropractic profession.
It is an amazing service that can help catch diseases and pathologies, it can be very helpful when looking for fractures, and it is fairly cost-effective for most situations.
But when does it begin to become an issue when everyone and their mothers are being put under X-rays when they go to the chiropractor?
We are going to be making this article very brief and to the point.
X-rays can be beneficial when necessary. Your providers that you are going to, that are relying on X-rays to treat you, are making you pay for unnecessary costs that will most likely not help your pain.
The American Chiropractic Association Has 5 Recommendations:
- In the absence of red flags, do not obtain spinal imaging (X-rays) for patients with acute low-back pain during the six weeks after the onset of pain.
- Do not perform repeat spinal imaging to monitor patients’ progress.
- Avoid prolonged or ongoing use of passive or palliative physical therapy treatments (such as heat, cold, electrical stimulation and ultrasound) for low-back pain unless they support the goal(s) of an active treatment plan.
- Do not provide long-term pain management without psychosocial screening or assessment for possible related psychological disorders, most notably depression and anxiety.
- Do not prescribe lumbar supports or braces for the long-term treatment or prevention of low-back pain.
How X-Rays Are Typically Used by Your Providers:
- X-rays to determine where to adjust
- X-rays used to scare people into prolonged treatment plans
- X-rays to monitor progress through the awfully long plans
- X-rays used to determine if the treatment plan got results
- X-rays used for additional ammunition to continue care if we did not see changes we wanted
Here are some fleeting thoughts for you all…
If your chiropractor needs X-rays to determine where to adjust, how do they know where to touch you if they are relying on the image to see where to go?
Perhaps putting your trust and investing your time, money, and efforts will be better spent on methods that will not rob you of your power and health!
Our skilled providers can easily manage and evaluate where to provide intervention without the need for X-rays and you typically get better results faster. Our focus is on you not what some snapshot image says about you.
Keep up the great work and LIVE LOUD!
Share with a friend or loved one.
5 Reasons Your Feet Hate You
5 Reasons Your Feet Hate You
It is sometimes crazy to think about your feet. I mean it is one of those body parts that just seem to be there. But when you consider that we are bipedal animals they basically do everything for us.
So here are a few reasons they are not too jazzed with how you have been treating them lately or for your whole life.
5 Reasons Your Feet Are Mad At You
1. You Never Give Them a Hug
When was the last time you touched your feet? I mean like grabbed that beauty pulled it in and gave it a nice squeeze. I bet the majority of you don’t even wash your feet all that well.
Ah, they are so far away.
We tend to forget that when we think about something our focus because more direct and intentional about those things and then it starts taking off from there. You start to realize that you have some sore points on the bottom, or a weird nail thing going on that you didn’t even notice before.
Now the point is not to focus on weird feet things that you may or may not have but more importantly, we are trying to get you to understand that your feet are a very important part of your body especially as it pertains to movement, health, and fitness.
2. You Force Them To Take Odd Shapes
I know we all know this but we basically turn a blind eye, and men and women are just as guilty to blame because some of the guy’s shoes out there that I have seen are crazy.
If your shoe comes to a point then your toes are pointing to you the middle finger!
We are not just talking about the front of the shoe we are also throwing in their heels, width, arches, all of it!
Now stop freaking out, cause I know ½ of you right now are thinking, “well I have flat feet” or “my arches are too high and they need support”.
This is not a one shoe size fits all conversation! (hey ooooo)
But one might argue that your feet are now this way because of what you did to them in the past. Neither here nor there we are trying to progress forward and not reminisce too hard on the past and what we could have done differently.
BUT!!!
All we are saying is that if you try to put a soft peg in a hard square hole eventually that peg will change its shape to fit in the constraints in which you are forcing it in.
Ideally, you want to have enough space in your foot wear for your foot to mold and adapt and change based on the various tasks and demands you are putting it through. Something as simple as walking required the middle part of the foot to splay out and spread to help disperse forces, all while transitioning from various positions of supination and pronation.
All of the micro-movements, although mostly unconscious mostly because we are disconnected from our feet see bullet #1, control lower limb positioning above, hip function and movement, pelvic alignment, and so on and so forth.
3. They Never Get a Massage
We could really argue this for our whole bodies. Most of us do not give ourselves the TLC that we deserve.
But with the shoes, you wear, walking throughout the day, sports and activities we do, the feet take a good beating!
Something as simple as taking a tennis ball, lacrosse ball, spikey ball, edge of a coffee table, really whatever you want and pushing and poking and digging in can create a massage session for your feet. This can reduce tight muscles and tension throughout the feet.
It will also improve joint mobility and motion which is absolutely critical for overall function of the feet.
Not to mention all of the benefits in proprioception you get afterward. Just touching an area of your body brings more awareness to the area, more awareness creates better mind to body connection which is what proprioception essentially is. The more aware I can be the better I can manage and operate that area of my body.
4. You Suffocate Them
I am very surprised by how many people I work with who report wearing their shoes for literally 95% of the day.
They wake up and spend maybe 30 min to an hour barefoot or in socks and then throw shoes on and do not take them off until they are getting ready for bed.
Let those puppies breath!!!
Have you ever tried to do a squat or bend down towards the ground in a new pair or jean or some kind of tight clothing? Your hips and knees cannot bend and move and they should and thus your ability to move is altered and changed.
The same is true for your feet in your shoes. If they do not have the simple spacial capacity to move when we are weight-bearing then the joints will not be able to move and ultimately start giving you issues. On the performance side, we need the toes to be bending and spreading out to ground us and distribute force adequately among the whole foot.
The better the distribution the more balance we have and more balance equal more control and we could argue that better control can lead to efficiency and performance.
5. They Don’t Live To Their Full Potential
As with most of our joints, our feet do not live up to their full potential.
What do we mean by this?
We use them in a very limited capacity and they are not able to do what they have the ability to do. Even if we are considering wearing shoes in which the feet are somewhat limited, depending on the type of shoe, we are not doing things barefoot.
So what do we suggest.
Find times and opportunities especially around the house or your yard to start wearing your shoes less and play and move with your dogs or your kids to challenge your feet, to make them stronger, to mobilize them and keep all of your joint healthy.
As we have stated many times in our articles motion is lotion, the more mobile and free we can keep our joints the healthier they will be, the better they will perform, and they will feel amazing!
So kick off those shoes and live a little!!
What is Sciatic Nerve or Sciatica Pain?
What is Sciatic Nerve or Sciatica Pain?
Everyone has an Uncle Frank! You know Uncle Frank, the uncle who when you politely ask, how have things been going, responds with: “OOOOH my sciatica has been acting up again.” As if it was a chihuahua that has been getting into the trash to dig out a taco bell bag and they cannot figure out why it would be doing such a thing.
But just like Uncle Frank, most people are somewhat confused when it comes to the term sciatica and what it actually means or what the symptoms actually are.
So we will run through and give you everything you need to know about sciatica and what you may be able to do if you think you may have it.
What is Sciatica?
When someone refers to their sciatica acting up they are really referring to their sciatic nerve. To simply say my sciatica is acting up is no different than saying my back is acting up. Well is it your upper back? Your lower back? You get the point. They are simply stating a known buzzword or phrase that has little to no context.
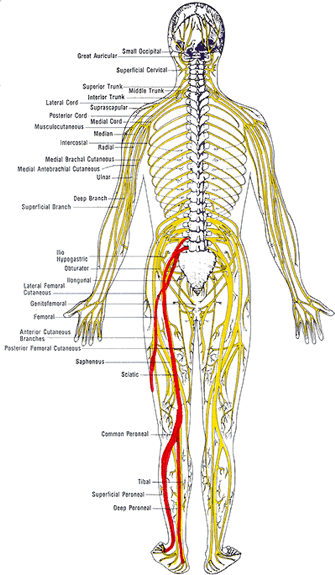
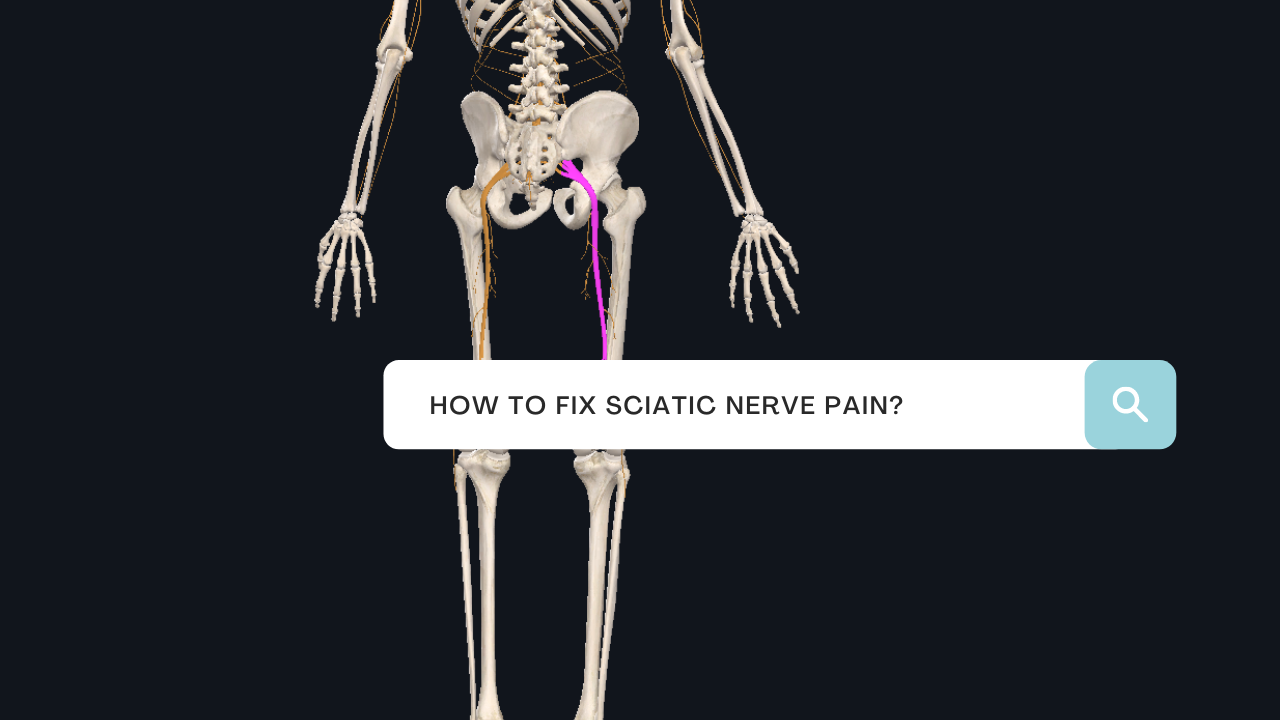
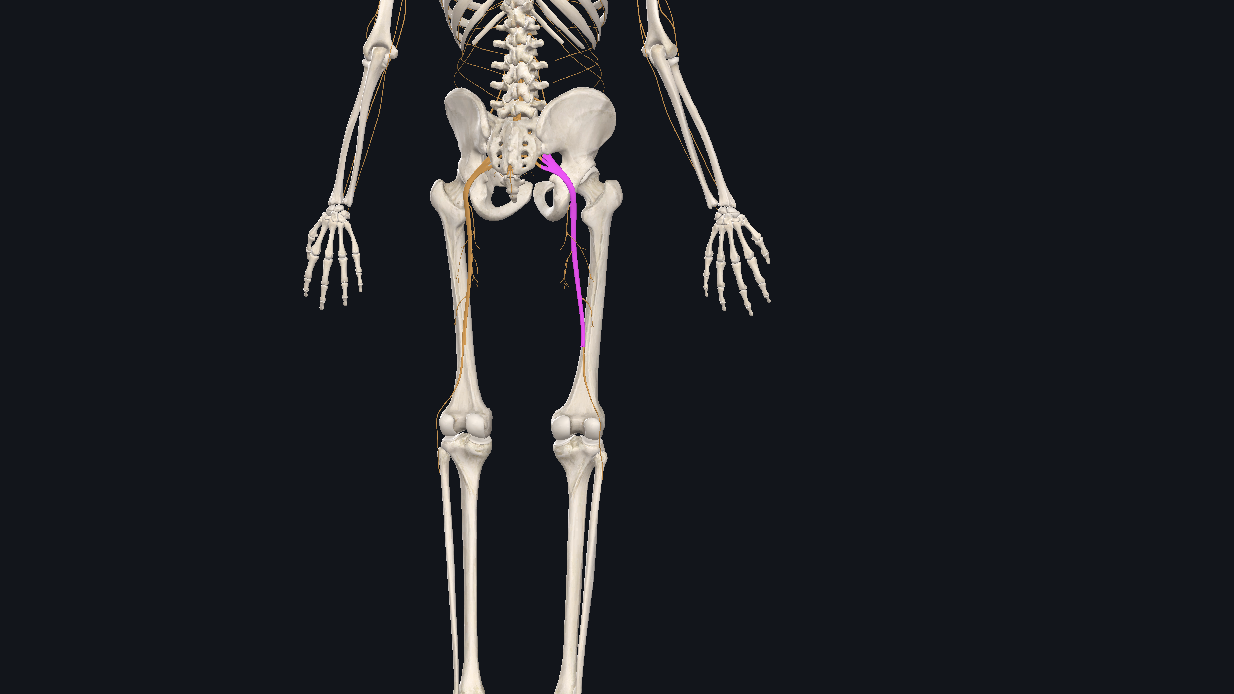
The sciatic nerve is one of the largest nerves in your body that is comprised of a number of lumbar and sacral nerve roots that exit the spine and combine into one larger nerve. When evaluating the image of the nerve we can see how the different levels of the spinal nerve roots blend together to form the sciatic nerve. This is important to understand as we will highlight how this helps determine the origin of irritation or pain for someone who is dealing with these symptoms.
The sciatic nerve then travels along the pelvis on each side and will begin to branch off into various different nerves that supply motor and sensory function to the lower extremity or legs. This too is also very critical information that will provide a great clinician detailed information about what and where there might be an underlying cause to your pain, numbness, or weakness.
As the nerve continues from the pelvis it runs along the back of the legs following the hamstring muscles to the back of the knee. What if tight hamstring muscles are really a result of a tight nerve? This may create valid arguments as to why tight hamstrings are not necessarily the cause of lower back pain but a response to the pain and a generator of guarding and protection.
A brief comment on the anatomy of nerves. Nerves like any other tissue structure in the body are compromised of cells and these cells require nutrients and oxygen just the same. And the also respond the same when their blood supply is occluded or compressed. Interesting enough because their operational functions are critical for many different functions throughout the body, it does not respond well when they are irritated.
In our office, we commonly portray the picture of the irritated friend, who that would otherwise be cool when planks are played on him now will all of the sudden lash out and overreact because he was already irritated. These normal stimuli that would not evoke a response have now set off a cascade of furry and fire! Internally our nerves are operating at a very similar capacity. If they are irritated through a chemical response, physical compression, or too much tension any simple act such as even putting on your socks and shoes can create an inflated pain response.
This concept is absolutely critical when trying to tease out the correct responses one should be trying to imply in order to seek recovery and reduce their overall pain sensitivity. Because the more you are in pain, the more pain you will be in.
While there are still some minor differences in opinion as to the the true definition of sciatica or sciatic pain there are some publications that have done the work for us to include some of the inclusion criteria for classifying sciatica. In the article “Clinical diagnostic model for sciatica developed in primary care patients with low back-related leg pain” in PLOS ONE 2018 authors have provided us a clear scoring table to predict the probability of sciatica. Reported symptoms in the studies were: reported pins and needles or numbness in the involved lower limb, reported pain below the knee, leg pain that is worse than their back, they had a positive straight leg raise test and/or femoral nerve test and/or slump test, and did they have any myotome (muscle) / reflex or sensory deficits in the lower extremity.
Based on the sum score as seen in the table in the article HERE one could then determine the probability of having sciatica.
This does not indicate the exact cause of the pain though it simply classifies where the pain is, although we may have some insight as to what the driving cause is from the history and intake questionnaires.
Based on who your provider is and their background will always have a slightly biased direction as to what they believe the underlying cause is, and that is why a full examination and provocative testing is best done to complete the evaluation and determine the best course of action. Based on the above symptoms you can see that some individuals can present with different types of symptoms and different locations of symptoms making this somewhat of a challenging issue.
More importantly than anything it continuing to have a conversation with you the patient to determine what were some of the activities we were or were not doing at the time the pain had come on. This may provide your clinician with valuable information as that what you should be doing and potentially not be doing. This also bridges us into what you want to be doing.
More often than not the fix or relief for these symptoms is found in the directional preferences of movement and the short term avoidance of others.
For example: Let’s say Uncle Frank’s lower back was sore from shoveling snow from a recent snowstorm. It was a heavy storm and he was hunched over for a period of time and now he struggles to put on his boots, socks, and pants. When he flexes forward he aggravates the nerve roots that were pissed off from the shoveling and now he is in more pain. But through guided movement therapies, we help Uncle Frank learn how to hip hinge more appropriately and reduce excess loading in the lumbar spine and improve the shared loading into the hips, all of the sudden what appears to be the exact same movement had reduced the patient’s discomfort and allowed them to improve their function. So the directional preference, in this case, was avoiding flexion of the spine when bending forward. This overtime will eventually not be the case but while things are sensitized it is wise to follow these preferences to help reduce pain and allow for faster recovery.
Let’s review the main way nerves get pissed off or irritated and cause us pain:
- Compression
- Tension
- Chemical
There are other pathological reasons for nerve irritation but we are focused primarily on functional and biomechanical alterations that would create your symptoms.
You will not always know that you have an irritated nerve though as many of the symptoms are different and occur in different areas for individuals. Here is a list of common symptoms:
– Radiating pain down the arm or the leg
– Muscle guarding, spasm, or cramping
– Numbness
– Pins & needles
– Aches that do not ease with pain medication
– Difficulty finding a comfortable, pain-free position
– Latent pain/tightness in response to stretching, posture, or activity, and
– No pain, but a tightness that does not loosen up (e.g. in the neck, back, hamstrings, etc.)
In our case for the sciatic nerve, you will see these symptoms occurring as high in the hip or glute/butt muscles and down all the way into the toes.
What to do if you have an irritated nerve?
Try not to piss it off more!
Easier said than done right? It is really about paying more attention to when you have symptoms and what was done prior. For some, it might be that you were literally not doing anything. Sitting and not moving might be aggravating depending on how much tension or compression is in the nerve. This is why it is important to have a proper evaluation and consultation with a professional.
With the sciatic nerve one of the most common complaints, is either a tight hamstrings or tight calf muscles and this prompts individuals to throw a leg up or start stretching these areas to only irritate things further. If it is a lumbar root driver, then prolong sitting or driving will commonly aggravate the symptoms.
How we work through this pain in our office:
- Directional Preferences
- Hip Hinges and Spinal Hygiene
- Passive Lumbar extension (McKenzie Extensions)
- Neural Mobilizations
- Lifting Weights and Resistance Training
- Directional Preferences
As mentioned above you want to understand and determine what directions are not responding well to the patient and find the positions that offer relief and or reduce symptoms. Progress is not always zero pain but also simply reduce symptoms or less pain down the leg. When the pain is relieved through these directional preferences we are taking either compression off of the nerve allowing it to reperfuse with blood and reduce chemical irritation, relieving compression forces and reduce signal transmission, or putting slack in the line reducing irritation. And the more you can offer this to the nerves the better they will respond.
1. Hip Hinging and Spinal Hygiene
Being able to hip hinge will have great carry over to any and most aspects of life as it affords you the ability to carry out functional tasks most efficiently as you learn to balance the load between the low back and the hips. When we can hip hinge the glute and hamstring are more involved reducing the amount of tension also put through the passive structure and nerves. This will also relieve any excess tension or pressure that might be pushing through the discs and causing nerve root irritation
2. Passive Lumbar extension
Many times the directional preference that responses best for individuals with sciatic nerve pain is the extension of the lower back. This is from McKenzie’s work and the active care model approach of self-managing your pain. These can be performed as press up or hip drop, but the key is to keep the low back muscles and butt muscles passive and relax. This will help reduce lumbar disc bulges and herniations, as well as put slack in the nerve roots, and give the guarded muscles and opportunity to relax. This tool is so powerful it is often overlooked. It is also recommended to be used throughout the day to relieve tension or tightness from prolong sitting.
3. Neural Mobilizations
Neural mobilizations are also referred to as nerve glides or nerve flossing. The intention is to keep the nerves mobile and sliding through the sheaths that surround them. Connective tissue restrictions can create kinks or binding restrictions that pull on the nerve creating more irritation. This may also be a result of inflammation accumulation from an injury that we want to try and maintain neural mobility. These should be done under the guidance and instruction of a professional as it is easy to put too much tension in the nerve and aggravate it further.
4. Lifting Weights and Resistance Training
We want to try and maintain as much of our functional capacity as we can through this time and there is no other best way than adding some resistance training. Resistance training will stimulate the body to continue adapting and recovering. It helps solidify technique and form. Most importantly if provides contextual feedback for how the body is feeling in real-time. If you are able to perform, lift, or do as a task without discomfort or pain then your body and nervous system will start to put together the pieces that your body is doing well and that you are not falling victim to these symptoms. The less you are in pain the less you will be in pain and if you can do that with challenging tasks then even more power to you!
Conclusion
The intention of this article was to provide insight and guidance into the most common causes of sciatic nerve pain or “sciatica”. This was in no way intended to diagnose your symptoms and what is causing the pain. There are other opportunities that may create similar symptoms and it is always suggested that you schedule a consultation and evaluation with a professional.
I’m Dr. Antonio with Live Loud Chiropractic and Coaching in Lafayette, Colorado. If you have any questions I am more than happy to help answer what I can and you can always call my cell phone number. 303-520-8974
Grease the Groove To Get Strong
Grease the Groove To Get Strong
Hi, my name is Dr. Antonio with Live Loud Chiropractic and Coaching in Lafayette, Colorado.
Today, I want to share a concept called Greasing the Groove. Greasing the Groove is a concept first shared by Pavel Tsatsouline with Strong First.
Oftentimes we have patients saying they’re struggling with a movement, or that they just don’t feel strong. It’s challenging because they’re often trying to complete a lot of reps within an hour training session. People tend to fatigue really fast, especially if it’s a movement they’re not very strong in at first. They’re not able to actually get good quality reps. You will find that you are fatiguing faster than you can get stronger, and you’re not able to build and train that strength.
PLAY VIDEO ⬇︎
How To Grease the Groove
As the story is told, Pavel had a pull-up bar hanging from the entryway into the kitchen. And every time he went into the kitchen, he did one pull-up. So throughout the day, with the amount of times he went through the kitchen, he accumulated a lot of reps.
The idea here is to be fully rested and prepared for the next set. So if throughout the day, for example, you do one pull-up every hour, you’re going to accumulate upwards of 16 to 18 reps, with every single rep feeling easy. So let’s say for after a week, you now have X amount of repetitions. As you start to feel stronger, you can continue to build up.
For me, I’ve been wanting to get my pressing strength back up in my pull ups. In my office, I have a pull-up bar and a kettlebell. And in between patients, I’ll do easy reps—reps I know I can complete and that I will not fail. And throughout the day, I get a ton of repetitions. And as I start to feel stronger, I’m going to add repetitions. To start, if I feel like I can only do one quality rep, I’m only doing to do one rep. I’m not trying to grind out extra reps just because I feel like I need to—I’m going to stop before I fail. But that doesn’t necessarily mean using “easy weight”—they’re easy reps, but you’re challenging yourself with a high stimulus type of weight.
As I get better at pull ups, I can’t stay at five reps and assume I’m going to continue to get stronger. I might have less rest in between those breaks, which allows me to get more volume. Or if the volume (how many sets I can do throughout the day) stays the same, then I might need to add repetitions or add weight to my body. There’s a lot of different ways that you can do this, depending on the time and equipment you have.
Conclusion
So there you have it! Greasing the Groove. The neurological patterning around that movement is enhanced and expanded, which helps make you stronger. A lot of this is neuro-driving and neuro-grooving. The muscles get a lot of repetitions and a lot of volume, and that results in building strength and muscle.
Keep up the great work and Live LOUD!
Share below with a friend or loved one!
How to Manage Low Back Pain During Pregnancy
How To Manage Low Back Pain During Pregnancy
Low back pain is incredibly common during pregnancy. I have so many women asking me, “how can I relieve my low back pain during pregnancy?” Oftentimes, this pain shows up when women are sleeping. It’s estimated that it can affect up to 80% of women at some point during their pregnancy, whether it starts in the first, second, or third trimester. And for 10% of women, it’s really severe. Women who have had a history of low back pain present the biggest risk of having low back pain during pregnancy.
I’m Dr. Nichelle Gurule with Live Loud Chiropractic and coaching at Lafayette, Colorado. Today I’m going to share some ways to relieve low back pain during pregnancy.
PLAY VIDEO ⬇︎
Managing Low Back Pain During Pregnancy Start With Understanding What Causes It.
There are so many changes that have happened to the pregnant body throughout the 40 weeks, and one of them is the structural changes that we all know about.
As the baby is growing obviously the belly is growing, and this will start to create a larger lumbar curve. With this, your posture changes, and the center of gravity is changing, and our low back muscles start working harder. The muscles are trying to anchor and hold on, so mom doesn’t fall forward.
There’s also additional weight gain that the joints aren’t used to handling in the back, hips, and knees. We have hormones that are all over the place—relaxin and progesterone are loosening up the connective tissue. This causes the ligaments to not do their job as well because they’re lax because of relaxin. We need them to do that because we want that pelvis to be able to expand for birth. However, when it does that, all the ligaments are lax, and now the muscles will grip on to compensate and hold the area stable.
So we talked about it a lot with the pelvis, but especially in the low back, if all of these little ligaments in here are relaxed, these muscles are going to grip on.
We also have an abdominal wall that is lengthening. Our core isn’t as strong as it was because of that lengthened position. We might have the abdominal wall beginning to separate, which is called diastasis recti, which is common; it will happen in 100% of pregnancies by 35 weeks.
But the truth is that the abdominal wall portion of the core is just not quite as strong to hold us in a good position and support the whole core unit. Intraabdominal pressure changes when you have a lengthened abdominal wall—you are no longer stacked, you’re angled—that changes how that pressure system is working. And in an ideal pressure system, everything is balanced: the abdominal wall, pelvic floor, the diaphragm is nice and balanced. But when you have a baby filling up that space, that core pressure system is changed a little bit.
And then last but not least, we also have a lot of emotional challenges during pregnancy. And that can play a big role in the aches and pains that we’re having.

How Can You Relieve and Manage Low Back Pain During Pregnancy?
As a chiropractor specializing in prenatal postpartum care, I recommend chiropractic. One of the reasons is that we reduce any restrictions that you might be having. And when you have an area of the body that’s restricted, the nervous system is not functioning as well to that area. So if you can imagine it, when a little area of the body is not moving well, it can’t send as many messages to the brain as to what’s going on. So the brain is just guessing as to what’s happening to this region of the body.
So we want to be able to get all of those joints and all the body into homeostasis so that as much good impact and feedback can come to the brain. We want to increase that nervous system function. By getting rid of any joint restrictions, we can get those tight muscles and tissues to relax.
We’re creating balance in the pelvis, in order to avoid a chain of problems. So chiropractic care can be really vital service for your pregnancy aches and pain.
Here are some things to think about when trying to manage your low back pain during pregnancy.
1. Posture
How are you sitting at work all day long? Are you slouched, tucking that sacrum back? Or are you on your sits bones? Chances are that you’re slouching at some point in the day if you’re at a desk a lot, or seated a lot, because you’re tired, and your core is weaker. So we want to have a back support behind us, and trying to sit on our sits bones, to help our back, our pelvis, and for the position of the baby. Because if we slouch, that can pull the baby’s back to our back due to gravity. We want to be on our sits bones to help that baby get in a bit better position and keep this space open for the baby. Slouching down doesn’t give as much space for the baby.
The car is really important. If you’re in the car for more than 10 minutes, you should have back support. I love the Back Vitalizer, but if you don’t want to buy something, roll up a bath towel, and put it behind your back.
How do you stand? Imagine there’s a string of the top of your head pulling you up nice and tall. And how are you lifting? Are you rounding to pick up a toddler? Are you rounding to pick up your bag? Focus and learn to hinge, and squat, or do a sort of lunge-squat coming down. The way you lift will really play a role in this as well, and especially in the postpartum, so building those habits during pregnancy is key.
2. Deep Core Engagement
So as you do things, activate your pelvic floor, activate your transverse and if you don’t know how to, go onto my YouTube videos that show you and talk to you about cues to activate those areas of the body specifically to activate the pelvic floor, activate the transverse, and then lift with that hinge or that squat. So learning how to activate that deep core is gonna be really important. That’s something your prenatal specialist or chiropractor should go over with you and teach you how to do that.
3. Sleeping With a Better Pillow Setup
I suggest people sleep with a pillow at their head, and a knee pillow. The knee pillow keeps the hips in line and keeps them balanced so that all night long, so they’re not collapsing down and impacting the pelvis and the low back. How we sleep matters, so let’s make sure we find the right setup.
4. Heat and Cold Treatments
Some people like heat more, some people like cold more—find what works for you. An Epsom salt bath is great because it gives you pain relief from the heat, but then the magnesium can help the muscles that are tight. Magnesium is great. Take magnesium orally, or get it through your skin in an Epsom salt bath.
5. Supportive Belts
Sometimes a supportive belt going under the belly and pulling up helps a lot. A SI belt is one that squeezes your hips and helps stabilize them. Not only does that help with pelvic pain, but it can also help with low back pain as well.
6. Ditch the Heels
If you’re wearing heels, that’s going to make more of a curve in your back, exacerbating the issue. Ditch the heels, even if they’re only little ones. Wear flats.

Best Movements for Managing Lower Back Pain During Pregnancy
Exercising is critical.
They increase blood flow and get things moving in the right way.
So what are the best exercises to do?
- To start, make sure that when you’re on your walk, you think about that string pulling you up, so you’re nice and tall during your walk.
- Good Mornings really work on that hip-hinge pattern and strengthen your back and glute muscles.
- Glute Meade activations. Put a band around your knees and do lateral walks, or come down on the ground and do glute bridges or clams.
- Stretch your glutes. Do something like an elevated pigeon, or a happy baby to stretch out your hip flexors.
- Try trigger point ball work to roll out muscles that are tight.
This is not a full-encompassing exercise routine here, but those are just some ideas that some of these exercises can work toward strengthening the deep stability muscles, or maybe the big meaty muscles we want to turn on.
Perhaps stretching will be more helpful for you…
We are able to strengthen with exercises and rehab, but sometimes stretching certain areas that need stretching can provide great relief for you.
BUT I will have a caveat that if you’re hypermobile or if you’re somebody who is super flexible, stretching may not be for you. So this is where an evaluation is key because, for some women who are pregnant, stretching can be detrimental and actually worsen the problem. So it’s really important to know if you’re somebody who should, or maybe shouldn’t, stretch during pregnancy. Exercises and rehab are going to be dependent on each person, but there’s a lot out there to help you with your low back pain.
Conclusion
This is not an exhaustive list for management and relief but something to also consider are the various services that you can seek help through.
Chiropractic paired with acupuncture is going to help get that body to homeostasis, as well as work on relaxing those tight muscles. So the combination of Acupuncture and Chiropractic can be incredibly beneficial, and massage as well.
There are a number of bodyworkers that can be helping you in addition to chiropractic.
Now again we know this list is not complete as different symptoms changes per person and also between pregnancies, but this is what we have found to be the best solutions for so many women on how to manage and relieve their low back pain during pregnancy.
Keep up the great work and Live LOUD!
How To Heal a Bulging Disc
Bulging Disc: How to Heal Low Back Pain Naturally & Make a Comeback
When it comes to understanding bulging disc, herniated disc, and other disc injuries that cause back pain, there are some nuances that’ll make it easier for you to heal naturally and make a comeback.
This is Dr. Antonio with Live Loud Chiropractic & Coaching in Lafayette, Colorado. Today, we’re going to cover exactly what bulging discs and herniated discs are and how they cause back pain. Most importantly, we’re going to cover how you can protect yourself from disc injury and what you can do about it if you’re already in pain from a bulging or herniated disc. If you have back pain or you’ve been told you have a disc injury, this blog will be especially useful for you.
PLAY VIDEO ⬇︎
What Are Discs and Vertebral Bodies?
When we’re talking about bulging or herniated disc, it’s not a black or white issue. So first you need to understand certain functions, how certain body parts move and operate, so you better understand your injury. The best way you can do that is by having a proper one-on-one evaluation, but this blog is going to help you immensely in the meantime.
To begin, the disc is what resides in between two vertebral bodies. The vertebral bodies form a column. The spinal cord goes down the middle of that column. It’s protected on the backside by the spinous processes, which is the spine that you can actually feel on your back. And then on the front side are those vertebral bodies. And those vertebral bodies stack up really nice like a column. And that column is what gives structural support to your spine. So when looking at the vertebral bodies, the discs are in the middle of them.
You also have nerve roots that come out from between two vertebral bodies. The nerve roots are what go out to your body, to your trunk, your digestive system, your extremities, so on and so forth to every inch of your body. They direct motor function, carrying signals going out that tell your body to do certain things. They also bring in information to the spinal cord and up to the brain.
You can think of the disc in between as the shock absorbers or the compression component of the spine, as it sits in between those two vertebral bodies. Now, it’s a very strong structure, but it can heal just like any other soft tissue. This foundational information will help you understand how to fix back pain from a disc bulge or herniation.

What Are Intervertebral Discs Made Up Of?
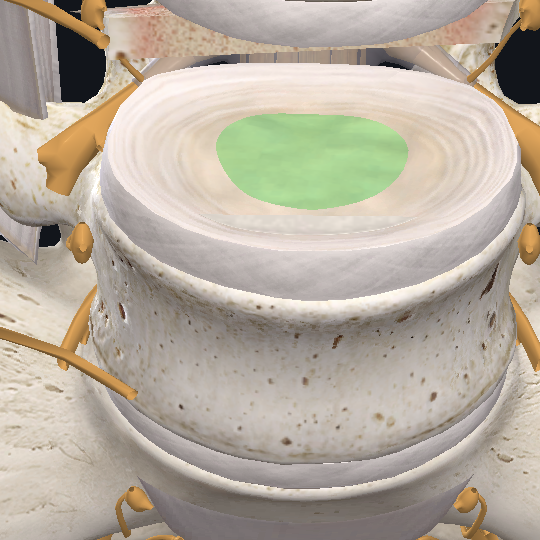
To better understand how a bulging disc happens, it’s important to know how the disc is made up. I want you to think of a tree trunk. If you look at an old tree trunk, you can see the rings, and the rings give you an indication of how old the tree is. But in the case of discs, the rings are called the annulus.
In a disc, looking from the top down, you’re going to have all these layers of rings that go from the inside and get bigger and bigger and bigger as they go around the outside. From the sides, you can imagine those rings lining up. But then the rings will also interchange and be at different angles going across each other.
So it creates this network or matrix of these annular rings that come together and can withstand a lot of great compressions. It also helps deflect twisting and rotational forces known as distraction forces. So any sort of force that goes into the disk is absorbed by this network and fiber of webs that pulls and compresses to make it very strong.

How Do Repetitive Movements Cause Annular Tears?
Now what happens in our day-to-day life is that you tend to do what we call repetitive movements or repetitive behaviors. So, for instance, if you work at a desk, you’re doing a lot of the same positions or movements. If you’re doing any sort of weightlifting or CrossFit or HIIT or even just working out in general, you commonly are doing the exact same motions over and over.
And if a formed technique or another number of factors that can happen begin to build up, then that same repetitive movement pattern wears on those annular rings. And you can get what’s called an annular tear. That’s the beginning of what leads to disc bulges and disc herniations.
Now, depending on the extent of the annular tear, you might not have a true bulge or herniation. You might just have symptoms from the annular tear, depending on where it’s located on the disc. There are three different regions of the disc:
- Middle
- Outer: The outer third of the disc where the actual pain fibers are
- Inner Nucleus: Fluid-filled center
If you have an annular tear without a bulge and you have pain, we do know that that annular tear is probably progressing or migrating towards that outer level.
How Does a Disc Bulge or Herniation Happen?
When talking about how disc bulge or herniation happens, force and pressure are important. Think of the nucleus of the disc as a jelly-filled donut. As you move, that nucleus is going to shift and migrate depending on where the forces are. It’s like a waterbed. If you push on one side of a waterbed, where does the pressure inside the waterbed go? It goes away from you.
That’s really important when we’re looking at disc injuries, herniations, and bulges because we want to know where the force is coming from and where the pressure is going. If you have an annular tear on the outside of the disc, for example, straight compressive forces might be fine.
But we do know from research that the compressive forces within the disc are higher when you’re sitting. And that pressure increases depending on how you’re sitting. As you start to flex forward, for example, the pressure pushes backwards. If you have an annular tear impacted by repeated compression, you’re going to start to see that disk swell into and push through that tear, creating a bulge or bubble on the backside of that disc.

How Does a Disc Bulge Cause a Pinched Nerve?
The bulging disc can actually push back into the spinal column. And depending on how that bulge pushes out, it might be bulging enough to where it puts pressure on a nerve root.
This is where you might get symptoms of sciatica down your leg. You might be feeling numbness or tingling. You might have a little bit of motor weakness or motor loss. Those would all be signs of a true pinched nerve. Oftentimes, when people get nervy pain, they refer to it as a pinched nerve, which may or may not be the case. But this would be an actual pinched nerve.
When your body starts to realize you’re getting this bulge, it’s going to activate the immune system in response to injury. This is going to bring a lot of localized inflammation to help clean up any debris left as a result of the injury, and you’re going to get more localized swelling. That swelling might put additional pressure on that nerve root.
So the pinched nerve might be the byproduct of the swelling in response to the injury, or it could be the disc bulge itself. All are important considerations when dealing with and rehabbing the injury.
Best Movements for Bulging Disc
There are certain movements that help with a bulging disc. To start, it can sometimes be helpful to use a steroid pack to reduce that localized inflammation. This provides you a lot of symptom relief and opens up a window of opportunity for you to do rehab care and movements. This supplements the treatment plan if you’re having a little bit of trouble gaining traction in your recovery.

McKenzie Exercises and Extension Based Movements
One of the best exercises for bulging disc is called the McKenzie extension. If you have a bulge putting pressure on the front side, for example, will push the bulge backwards. With the McKenzie or Extension based movements, you put pressure on the backside of the disc by going through an extension movement. This will actually put pressure into the back of the disk, helping to reduce that bulge or herniation as it migrates forward. This is why we use a lot of hip drops in our office.
Mindful Movements for Bulging Disc
The other thing you need to consider is how you’re moving throughout the day. Let’s say, for instance, you’re unloading the dishwasher. If you’re not hinging through your hip joint, you might add more flexion in your spine and put more pressure and bulging in that disc.
If you’re being super-mindful about how you’re moving, but then do something a little more careless by flexing your spine forward, it’s like having a cut on your knuckle that you’re trying to heal but then grab something so that scab cracks because it’s right at that flex point. And so it makes it very hard to heal that injury when it keeps moving.
This might be a time when you need to put a splint on your finger to not allow it to move so that scab can heal. The same holds true for this disc bulge or herniation. That annular tear can take a little bit longer to heal due to the nature of the blood flow and nutrient supply that it gets, but given time and careful movement, it can heal like other soft tissue injuries.
What commonly happens, though, when most people go through lower back injuries, disc herniations, and bulges is that they’re not focused on the preventative side other than just rest and don’t do anything. They might do some exercises, but they’re really just hoping it will heal with rest. What most people don’t realize is that the positions or motions they’re doing on a daily basis, activities of daily living such as unloading the dishwasher, picking up a bag of dog food, leaning over to wash your face or brush your teeth, are all opportunities in which you can help the healing process or hurt the healing process by scratching that scab that’s trying to heal.
Hip Hinging for Bulging or Herniated Disc
Properly hinging at the hip instead of flexing the spine is one of the best preventative movements for bulging or herniated discs. Your hip joint is a big ball. It’s a big greasy ball and socket joint. It’s really good at providing movement.
The spine, on the other hand, can move and is really good at flexing, but it depends on the load and the context of the task at hand. When you’re picking up something heavy or bending forward, you need to hinge better through the hip to reduce the load on the disk. This way the spine isn’t flexing and bending all that much. Instead, there’s a pivoting around the ball and socket of the hip, allowing the back to remain straight.
Hip hinging is a prime opportunity for you to keep doing all the things that you need to do, especially if you’re a parent, have a very active lifestyle, or just want to continue the activities you enjoy such as gardening. This movement allows you to stay active without continuing to irritate the disc injury and disc you’re trying to protect.
Prevention Goes a Long Way for Bulging Discs
These preventative measures are one of the most critical factors when trying to get over disc bulges and herniations. The way you develop a condition is commonly how you get out of it. So if you have poor movement mechanics from exercising or lifting at work, for example, then you need to be mindful about those things so that you can let the disc heal while also staying active. You also need to know these mindful preventative movements are what you need to work on going forward so you don’t reinjure the disc.
Again, disc bulges and herniations can and do heal. They often just need a little bit more time and effort. Most don’t know to make the necessary changes to their movement patterns. And they just keep irritating the disc. That’s why healing can get super frustrating. You think…Oh, it’s been a couple months and I’m not seeing any progress or things are getting worse.
If this is you, take a step back. You’re just forgetting that you have to be mindful of those movements patterns. Almost everyone sees some disc bulging or herniation from time to time. It can’t be avoided completely. But when you do get that little bit of pain, it’s an indication that the movements or activities you’re doing are causing too much disc loading and pressure.

Muscle Guarding With Bulging Discs
Now the last thing you’ll want to consider is, oftentimes, a lot of the pain you might be experiencing is the muscle guarding intention that comes as a byproduct.
It is very rare that you will actually strain a big, thick hearty muscle such as the QL. Yes, it’s possible when doing a lot of the movements that trigger or exacerbate lower back pain. But what we often at Live Loud Chiropractic headquarters in Lafayette is that pain is a byproduct in muscle guarding the nerves or the discs.
When you start doing a lot of activities or repetitive movement patterns that constantly irritate those structures, your body is going to say…This does not feel good. I need to lock it up and protect it so that things don’t get worse. And then you get a lot of lower back tension or tightness or spasms or guarding.
Imagine if I asked you to hold your bicep and squeeze it really tight. How would that bicep feel after a couple minutes, hours, days, or even a couple weeks? It’s going to start burning. It’s going to hurt because it’s constantly in the contracted state. When muscles are contracted, they also squeeze arteries and vessels that go through them and supply them with nutrients and oxygen. So the muscle starts to burn even more because it’s in a hypoxic state, and it’s not getting the actual nutrients and oxygen it needs.
The Feed-Forward Mechanism in Naturally Healing Disc Bulging
Now the last thing you’ll want to consider is, oftentimes, a lot of the pain you might be experiencing is the muscle guarding intention that comes as a byproduct.
It is very rare that you will actually strain a big, thick hearty muscle such as the QL. Yes, it’s possible when doing a lot of the movements that trigger or exacerbate lower back pain. But what we often at Live Loud Chiropractic headquarters in Lafayette is that pain is a byproduct in muscle guarding the nerves or the discs.
When you start doing a lot of activities or repetitive movement patterns that constantly irritate those structures, your body is going to say…This does not feel good. I need to lock it up and protect it so that things don’t get worse. And then you get a lot of lower back tension or tightness or spasms or guarding.
It’s important for you to find opportunities that allow the muscles that are guarding and protecting to calm down and relax in order to help the healing process. The more those muscles calm down and relax, the more you’re able to move. And the more you’re able to move, the more blood flow can get in to heal the area.
This will also allow you to realize that certain movements are actually feeling good.This is called a “feed-forward mechanism” or a “snowballing effect.” If you can get rolling in the right direction and gain some momentum, then, commonly, you’re going to keep that momentum going forward in a good way.
The Negative Feedback Loop In Naturally Healing Disc Bulging
The same is also true, though, when you start irritating it. If you’re not being conscious about the movements that irritated it in the first place or that cause more pressure on the disk, then you start having a negative feedback loop. The more pain you feel, the more pain you’re going to experience. And then the more pain you’re in, the more you’re going to become sensitized. Until you get to the point that any little movement or anything out of the norm is going to set you off and trigger more pain.
This is very common for a lot of chronic pain individuals. They just see this bouncing from…I’m good for a little bit, but then I get really bad. And then I feel a little better because I don’t do anything. And then I get really bad. They’re constantly in this flip-flop mode of too hot, too cold, too hot, too cold. In these cases, we really need to dive deep to discover what exact movements and activities irritate it, which it going to be different for everybody.
Making a Comeback after Disc Bulging, Herniation, and Injury
The biggest takeaway is that you need to find opportunities that allow you to move and keep moving. You need to look at the ways you can work on muscle tension and how you can move better. You should look at the ways you’re doing your exercise classes, your training, or working out at the gym. Those repetitive movements are all really important pieces of the puzzle. But there is not a one-size-fits-all approach. It has to be tailored for your body.
We do see a theme, though, with disc herniation and bulges. For many people, it’s that bending forward and flexing forward that tends to trigger them the most. So we have a couple of starting points that work really well.
First, if you have nerve pain or signals or symptoms, don’t just assume you need drugs or surgery. Movements and decompression are also very, very valuable. You just need to know the right exercises to do, and McKenzie extensions and hip hinges are a great place to start.
Next, if you are suffering from disc injury or you’ve been told you have a disc herniation bulge, do not write this off as a death sentence. There are a lot of things you can do. Your disc can heal itself. And even if it doesn’t do that completely, there are additional exercises to continue to strengthen your core and your hips. These can help stabilize and make your back stronger and more robust, which might have been the reason a disc injury happened in the first place.
Finally, if you have experienced disc injury, you know how tough it is. I hope this information helps boost your confidence while recovering from injury as well as preventing re-injury if you tend to have recurrent back pain episodes. And if you know of someone who’s dealing with a disc injury, please share this information with them.
Conclusion
Unfortunately, many of these things are not being taught by medical providers, orthopedics, or physiatrists. Even physical therapists are sweeping some of this under the rug, asserting that these basic movement changes don’t work. But they do. Now you understand how the discs work and can ask the right questions to figure out the right path for you to heal and get on with the adventurous life you are made for.
We’d love to hear your bulging disc or disc herniation questions and experiences. Comment below to tell us what has or hasn’t worked for your disc injuries.
Fixing Sciatic Nerve Pain
Fixing Sciatic Nerve Pain With 3 Easy Exercises
If you’ve ever suffered from sciatica, or pain that maybe runs from your back down into your legs, or you know someone who’s been through this before, you’ve seen how rough it can be, and this blog is going to be very valuable for you.
*Disclaimer this post is for educational purposes, consult with a clinician to determine the best course of care and movements for your pain, or reach out to us for a consult*
Today, we’re going to show you three basic exercises that you can do to help combat sciatic pain. First I will give a brief anatomy lesson about where your sciatic nerve is, and also discuss some of the common misbeliefs that are associated with sciatic pain, and how you can better approach it so that you can actually tackle it once and for all.
Hi, my name is Dr. Antonio with Live Loud Chiropractic and Coaching here in Lafayette, Colorado. Today, we’re going to be talking about relieving sciatic nerve pain!
PLAY VIDEO ⬇︎
Common Question About Sciatic Nerve Pain
- What are the best stretches that I can do?
- What are the best physical therapy exercises I can do for sciatic pain?
- What are the best stretches I can do for sciatic pain?
- Why do I only have pain on one side of my back and down into my hip?
- Why isn’t it the same every day and it changes?
- Why did I just get this sudden onset of pain into my hip?
And a lot of common places we see sciatica pain coming up is not necessarily all the way down the back of the leg as most of us might think. You might just be experiencing it right into your buttock region, or your hip region and a little bit down into your leg. And so there are some nuances there that are going to be very important for you to be able to determine what is the actual cause of the sciatic pain.
We want to be able to help you provide relief, but it’s difficult to ascertain and assess what your actual cause is.
If it is Sciatic Nerve Pain, nerves are very sensitive, and you don’t want this to turn into something more that will create more symptoms, more agitation, numbness, pain, or tingling.
What is the Sciatic Nerve?
The sciatic nerve is the big, long, thick nerve that runs from the front side of the pelvis where the lumbar nerve roots come, through the pelvis, and then runs down the backside. Now keep in mind, what you don’t see are all the tiny little nerves branching off that supply function and sensory components to the gluteal muscles.
So as we slowly add some of these muscle layers on, we have deeper levels of the glute this is the piriformis which often gets blamed for sciatica symptoms. But we believe it’s not as important as other issues.
Your glutes cover that, so a lot of times the pain in the hip is a sign of a pinched nerve. Likely something in the back is causing a pinched nerve and that’s why you’re getting symptoms that are referred down into the leg. From time to time, you can get sciatic symptoms that are all the way down past the knee and into the foot and into the lower extremity.
But more commonly, we see this happen in the hip. What I want you to take note of are the lower back structures. In between all the lumbar vertebrae, there are discs, and in between the discs, there are the nerve roots coming in and out of the spinal column. These nerve roots then come down together and create the sciatic nerve. This is where a pinched nerve often occurs, a lot more frequently than the classic piriformis syndrome that gets blamed.

Where Does the Pain Come From?
Sciatic pain is a very common diagnosis, and it is even more commonly misdiagnosed, as it is used as a general kind of region open for interpretation. But we want to be more specific with the diagnosis so that you can be very time efficient with your exercises. Usually, as we feel a pinched nerve, we would assume that the side of the pain is where the actual pinched nerve is. However, those tender points that you feel in the glutes and down to the leg might just be a symptom of the pinched nerve that’s up higher.
Many people are just rolling out and stretching and not getting the relief that they need and deserve, because they were improperly instructed. They don’t realize it’s actually coming from their back, but rather, they think it’s coming from their hip, or their piriformis, or their hamstring, or something like that. But if you start to pay attention to when your symptoms in your leg increase, I have a feeling that you’re going to also find that your lower back pain symptoms tension or whatever that might be, might also be increasing, which would be highly indicative that the pain is coming from the back and not necessarily the leg.
We wanted to explain this so you can understand why we’re giving you exercises specific to the lower back. There are methods and strategies that can help alleviate sciatic symptoms, but we’re talking about fixing, we’re not just talking about alleviating. Alleviating is putting a bandaid on it. But what we’re looking to do is actually find where the nerve is pinched, so that you can create solutions you actually need.
I hope you enjoy these exercises, which are going to be super helpful for you.
Best Movements for Sciatic Nerve Pain
1. Door Squats
Our first exercise is for those who are having sciatic pain and hip pain associated with lower back pain. Door squats allow you to offload the lower back into the hips, so that you can continue to move and not overload them where they feel like they’re only getting tighter.
Grab both handles on either side of an open door. Have a wide stance in order to maximize range of motion in the hips without flexing the lower back.
Then lean back like you’re water skiing so your arms take over most of the slack and weight. As you squat, use your legs, hips, and quads, as well as your arms to help guide you. Lean all the way back, using the best form possible, but also use the doorknobs to help keep your spine nice and straight.
2. Quadruped Hip Drops
Quadruped hip drops help alleviate all the tension in the lower back. It also works to help reduce any pain that may be caused by a herniated disc or pinched nerve that causes pain down the legs.
Start on your hands and knees, with your hands slightly in front of your shoulders. From there, shift your body forward, and gently let your hips sag to the ground in an “upward dog” position. Be sure not to force your hips down, but rather, let gravity guide you down as your arms prop you up. Repeat this back-and-forth motion until you feel some release.
3.Hip Hinge Movement
The constant motion of bending over not only puts tension on the sciatic nerve but also puts pressure on the lower back. Our solution is a simple hip hinge movement.
Every time you bend over, likely to pick something up around the house, be sure you’re bending and folding at the hips in order to maintain a straight long spine. This puts the weight into the hamstrings and legs, rather than the lower back. The hips simply go back and forth. Shift the hips, bend at the knees, and avoid loading weight in the lower back.
Conclusion
And there you have it!
Our top three exercises for fixing sciatic nerve pain. These are simple, but they’re so powerful. We hope you will find at least one exercise that works best for you. Take them step by step, inch by inch, But remember, it takes application. You can’t just do one set of 20 and be healed. If we’re assuming there’s an issue causing this, it’s going to take repetition multiple times a day, even once an hour, depending on what the severity is.
Take them step by step, inch by inch, and soon it’ll be a habit. But if it’s not creating a benefit, then we encourage you to seek external help and dive deeper into figuring out what will work for you.
Please share this with someone you know that is suffering from sciatic symptoms, and we hope that it brings you or them as much relief and benefit that it’s brought myself, and our patients here at Live Lab.
Keep up the great work and Live LOUD!